Reducing Stigma Towards Opioid Use Disorder Treatment

The repeated use of a substance that creates problems in a person’s home, work, or school life is defined as a Substance Use Disorder (SUD), a treatable mental health condition (Substance Abuse and Mental Health Services Administration [SAMHSA], 2020a). The United States (U.S.) loses nearly 185 people every day to substance overdose deaths (Hedegaard et al., 2020). Opioids are involved in almost 70% of the lives lost due to substance overdoses, equating to nearly 47,000 opioid-related deaths in 2018 alone (Hedegaard et al., 2020). Opioid Use Disorder (OUD) is a type of SUD defined by the repeated use of opioids (see the American Psychiatric Association for a more detailed definition of OUD; Dydyk et al., 2020). The economic burden of OUD and fatal opioid overdose is estimated to be over one billion dollars annually in the U.S. when accounting for healthcare and treatment, criminal justice, lost productivity, reduced quality of life, and value of life lost costs (Florence et al., 2021). OUD significantly impacts the lives of individuals who experience OUD, families and loved ones, and communities nationwide.
SUDs, including OUD, are among the most stigmatized health conditions in the U.S., despite the many evidence-based treatment options (da Silveira et al., 2018). Stigma carries with it a heavy weight, causing challenges for people who are stigmatized, such as reduced employment or educational opportunities, and marital or social problems (Corrigan et al., 2017a; van Brakel, 2006). Stigma prevents individuals with OUD from being able to access needed services or enter recovery, contributing to the thousands of lives lost every year to opioid overdose (Hedegaard et al., 2020). To better identify, understand, and eliminate stigma, this fact sheet discusses how stigma against treatment hinders recovery, evidence-based treatments for OUD, and strategies to combat OUD treatment stigma.
Stigma as a Barrier to Treatment
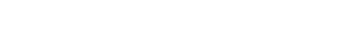
Stigma against people with OUD increases the harm experienced, creating a continuous negative cycle that may harm an individual’s recovery journey (see Figure 1).
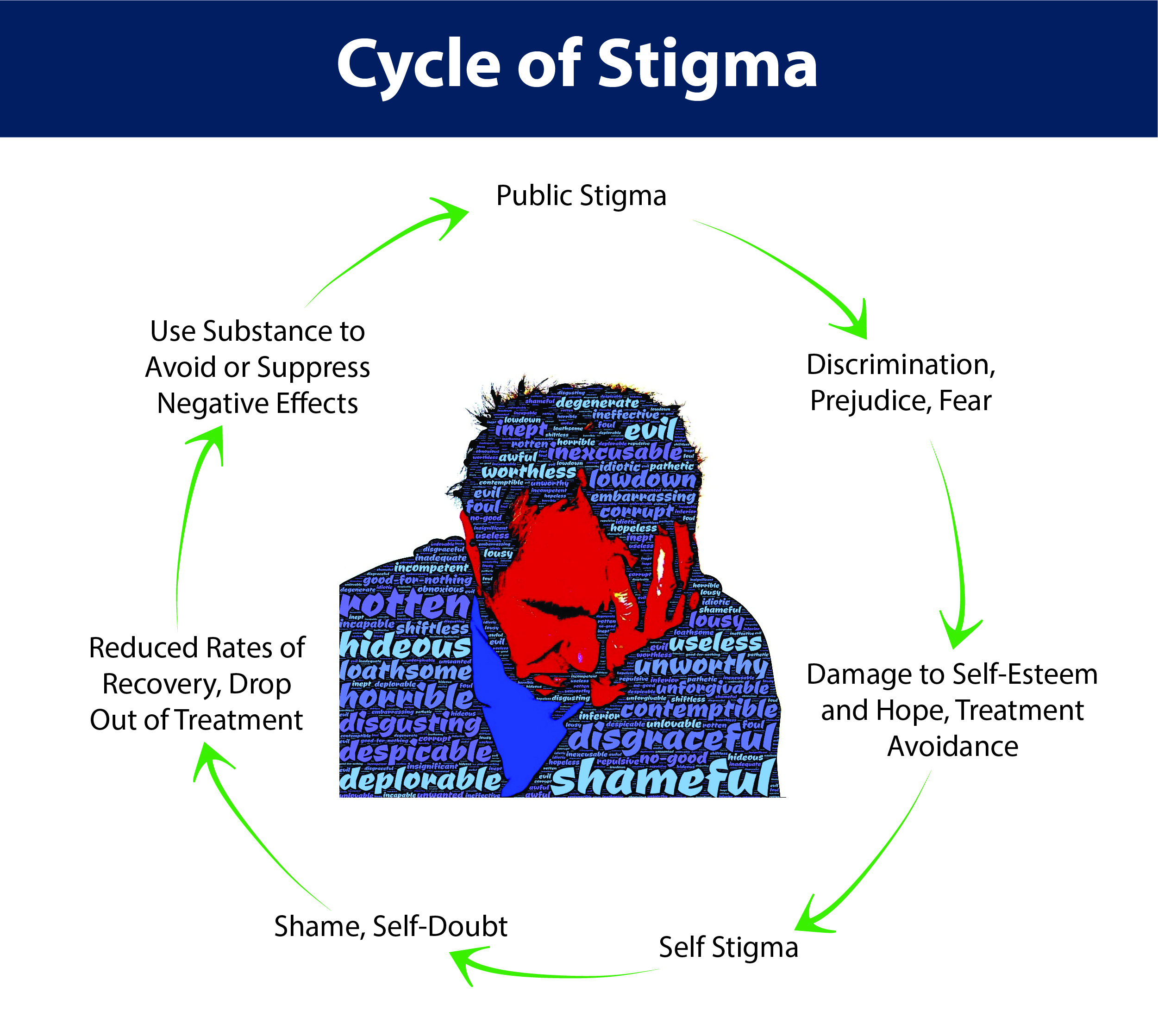
Figure 1: Stigma increases the harm felt by people with opioid use disorder, decreases the chances of entering and completing treatment, and leads to a destructive cycle (Corrigan et al., 2017a; 2017b; da Silveira et al., 2018).
Stigma is defined as negative beliefs about, and attitudes toward a specific group of people. Stigma is being “reduced…from a whole and usual person to a tainted, discounted one” (Goffman, 1963, 105). Stigma manifests in multiple ways such as public, structural, and self-stigma, all of which create barriers to obtaining treatment (see Figure 2).
Figure 2: Stigma creates barriers to treatment and many people who need treatment never get it. The pathway to treatment looks different for everyone and is not a straight line or linear process (Ashford et al., 2019; Corrigan et al., 2017a; 2017b; da Silveira et al., 2018; Luoma et al., 2014; McGinty & Barry, 2020; SAMHSA, 2020b; van Boekel et al., 2013).
Public Stigma
Public stigma is the negative views held by society about a group of people. It labels that group as “other” and views them as flawed and lesser (Corrigan et al., 2017a). Structural Stigma is the collection of negative views held by a society that leads to practices and policies that discriminate against the stigmatized group (Corrigan et al., 2005; McGinty & Barry, 2020). Self-stigma occurs when a person adopts and internalizes the public stigma held by the society around them and begins to view and label themselves in the same way that society does (Corrigan et al., 2017a).
All types of stigma create barriers between people with OUD and treatment. People with OUD may avoid seeking out treatment for their disorder to avoid being labeled and stigmatized (Corrigan et al., 2017b). Structural and public stigma decrease public support for funding substance use treatment services, thus making them less available to those who need them (Kennedy-Hendricks et al., 2017). Public stigma may also prevent treatment facilities from being built within communities, making it difficult for people to find local treatment options (McGinty & Barry, 2020). Public stigma may even impact the quality of health care a person receives (van Boekel et al., 2013). OUD stigma ultimately leads to fewer people being able to find, enter, and successfully complete treatment (Ashford et al., 2019; Luoma et al., 2014).
Evidence-Based Treatments* for Opioid Use Disorder
Learning about effective treatments for OUD is an effective way to reduce the stigma against OUD (McGinty & Barry, 2020). Successful treatment looks different for everyone and there are a number of effective treatment options available. Treatment should begin with a clinical assessment to establish a plan best suited for each individual.** The most effective treatments combine medication-assisted treatment (MAT) for OUD with psychosocial and/or behavioral treatments (SAMHSA, n.d.). A few examples of evidence-based treatments for OUD, not an exhaustive list, are presented in the chart below:
Psychosocial Treatments:
Used to help people learn to control desire for substances and avoid using substances while also teaching healthy coping skills for stressors or emotions (Dugosh et al., 2016).
| Type of Treatment | What it is | What it does |
|---|---|---|
| Peer Support |
Establishes a support system of nonprofessional peers with similar lived experiences. Examples: Alcoholics and Narcotics Anonymous, SMART Recovery. (Tracy & Wallace, 2016) |
Creates a safe, nonjudgmental space where individuals can feel a sense of connection and belonging. Effectively decreases substance use while increasing engagement with care. (Buckingham et al., 2013; O’Connell et al., 2020). |
| Motivational Enhancement Therapy (MET) |
Focuses on the exploration of the pros and cons of continued substance use versus changing substance use behaviors. (Miller et al., 1993; Prochaska & DiClemente, 1983) |
Can help individuals gain insight into substance use, increase individual motivation to change, and supports remaining substance-free. Effectively decreases substance use and subsequent return to substance use. (Cummins & Tobian, 2018; Rohsenow et al., 2004) |
Behavioral Treatments:
A specific type of psychosocial treatment that focus on the current problems a person faces, rather than past events, by supporting people through setting and achieving specific goals related to OUD (Association for Behavioral and Cognitive Therapies, 2020).
| Type of Treatment | What it is | What it does |
|---|---|---|
| Rehabilitation |
Occurs in various settings and formats, such as through specialized inpatient facilities, residential programs, or outpatient programs. Each is different in treatment time, duration, and structure. (SAMHSA, 2014) |
Combines training and services such as life skills training, substance use prevention training, and counseling services. Effectively decreases substance use when used in combination with other treatments. (National Institute on Drug Abuse, 2018; SAMHSA, 2014) |
| Cognitive Behavioral Therapy (CBT) |
Helps individuals understand the thoughts, feelings, and impulses that influence behaviors; teaches the skills to change negative thinking patterns and behaviors. (Gatchel et al., 2014) |
Individuals are taught to recognize triggers for opioid use and learn healthy coping skills. Effectively increases coping skills and decreases substance use. (Larimer et al., 1999; Roos et al., 2020) |
| Acceptance Commitment Therapy (ACT) |
Uses a mindfulness-based approach that focuses on being present and aware of one’s thoughts, feelings, and actions. Focuses on values and maintaining healthy behaviors. (Pollak et al., 2014) |
Individuals use thoughts, feelings, and emotions as tools to acknowledge, cope with, and manage OUD. Effectively decreases substance use, cravings, and impulsivity. (Lee et al., 2015; Pollak et al., 2014) |
How to Combat Stigma
The recovery process is facilitated by the help of supportive relationships (SAMHSA, 2020b). Here are some ways that you can combat stigma in your own life and help support people in recovery:
- Recognize that OUD is treatable and recovery is possible.
- Learn more about evidence-based treatment strategies for OUD.
- Support loved ones and encourage treatment (e.g., go with to appointments or give a ride, ask how things are going, provide a listening ear, etc.).
- Read or listen to stories from the opioid crisis, spread hope and healing.
- Acknowledge and understand the contributing factors for OUD.
- Learn and use person-first language (see Figure 3). (Kelly et al., 2015; Livingston et al., 2012; McGinty & Barry, 2020; McGinty et al., 2015; McGinty et al., 2018; Saloner et al., 2018; Yaugher et al., 2020).
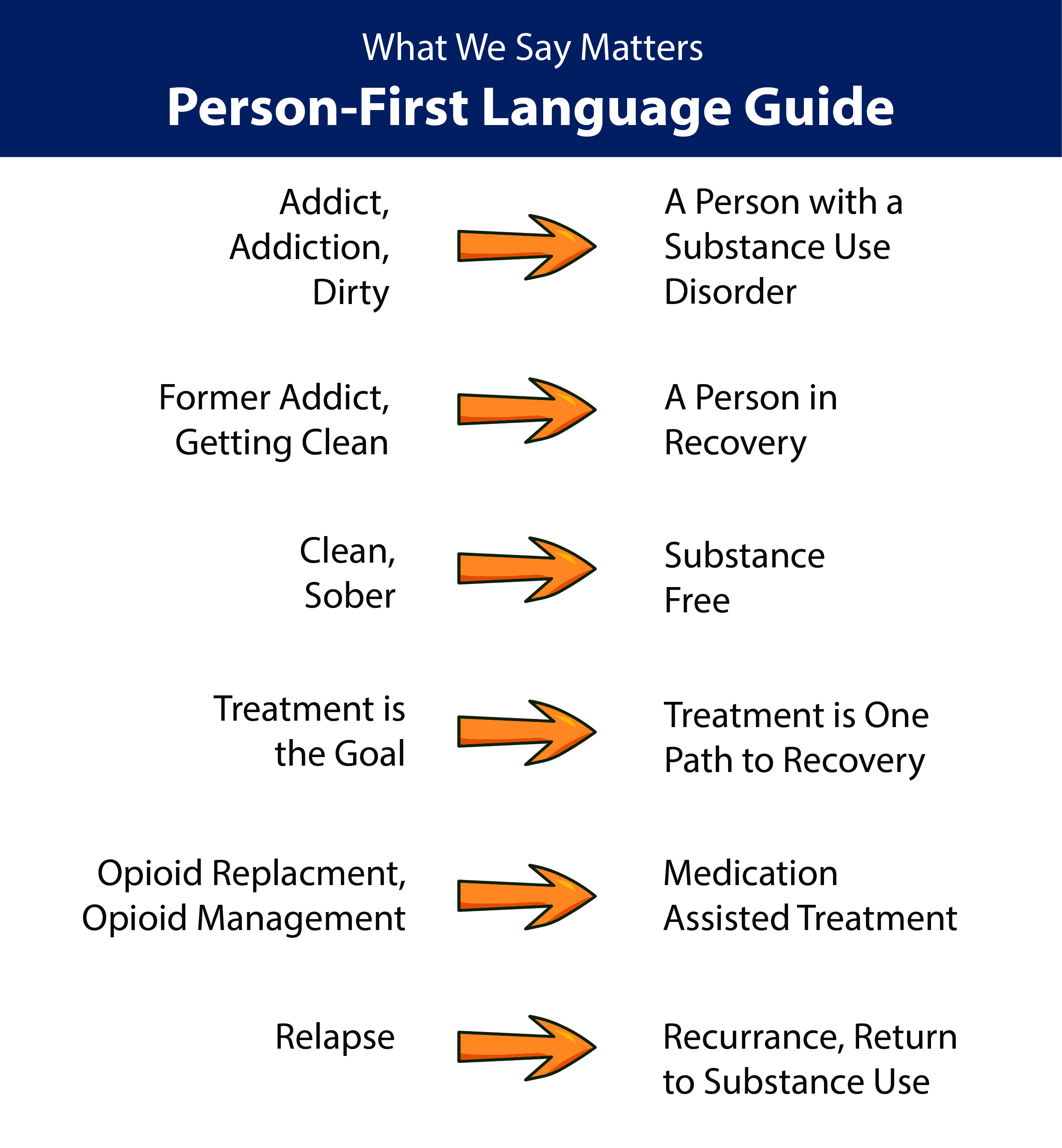
Figure 3: Replacing stigmatizing terms with person-first language is a good way to decrease the stigma against opioid use disorder (American Psychological Association, n.d.; Kelly et al., 2015; Kelly & Westerhoff, 2010; Yaugher et al., 2020).
Conclusion
Working to reduce stigma has many benefits, including saving lives and reducing other costs associated with the opioid crisis, such as loss of productivity and quality of life. There are many evidence-based treatments for OUD that support recovery and are highly effective. We all have a part to play to reduce stigma and can start by coming together to support treatment access and recovery. Reducing stigma saves lives, treatment works, and recovery is possible!
Disclaimers
*Always consult a trusted healthcare provider about what treatment methods are right for you.
**All of the information and resources provided here are for educational purposes only and this fact sheet should not be used to diagnose or treat any health conditions. Utah State University (USU) does not endorse or control any of the websites, books, or articles referenced.
Additional Resources:
- USU Extension HEART Initiative - www.extension.usu.edu/HEART
- Stories from the Opioid Crisis:
- Utah State University – Informing the National Narrative: Stories of Utah’s Opioid Crisis https://digital.lib.usu.edu/digital/collection/p16944coll134
- Utah Department of Health – Stop the Opidemic Stories - https://www.opidemic.org/stories/
- CDC Rx Awareness Stories - https://www.cdc.gov/rxawareness/stories/index.html
Fact Sheets:
- Reducing Stigma Toward Medication-Assisted Treatment: An Evidence-Based Overview of Treatment for Opioid Use Disorder - https://extension.usu.edu/heart/research/reducingstigma
- 10 Ways to Support Someone in Recovery - https://extension.usu.edu/heart/files/supportcard.pdf
- How do I Change My Language - https://extension.usu.edu/heart/files/stigma-languagecard.pdf
References:
- American Psychiatric Association. (2018, November) Opioid use disorder. Retrieved from https://www.psychiatry.org/patients-families/addiction/opioid-use-disorder/opioid-use-disorder
- American Psychological Association. (n.d.) Guidelines for bias-free language for disability in APA journals. Retrieved January 17, 2020 from https://apastyle.apa.org/stylegrammar-guidelines/bias-free-language/disability
- Ashford, R. D., Brown, A. M., Canode, B., McDaniel, J., & Curtis, B. (2019). A mixed-methods exploration of the role and impact of stigma and advocacy on substance use disorder recovery. Alcoholism Treatment Quarterly, 37(4), 462-480. https://doi.org/10.1080/07347324.2019.1585216
- Association for Behavioral and Cognitive Therapies (2020). Opioid use disorder [Fact Sheet]. Retrieved from https://www.abct.org/Information/?m=mInformation&fa=fs_OPIOIDS
- Buckingham, S., Frings, D., & Albery, I. (2013). Group membership and social identity in addiction recovery. Psychology of Addictive Behaviors 27(4). doi: 10.1037/a0032480
- Corrigan, P., Kerr, A., & Knudsen, L. (2005). The stigma of mental illness: Explanatory models and methods for change. Applied and Preventive Psychology, 11(3), 179-190. https://doi.org/10.1016/j.appsy.2005.07.001
- Corrigan, P., Schomerus, G., Shuman, V., Kraus, D., Perlick, D., Harnish, A., Kulesza, M., Kane-Willis, K., Qin, S., & Smelson, D. (2017a). Developing a research agenda for understanding the stigma of addictions part I: Lessons from the mental health stigma literature. The American Journal on Addictions, 26(1), 59-66. doi: 10.1111/ajad.12458
- Corrigan, P., Schomerus, G., Shuman, V., Kraus, D., Perlick, D., Harnish, A., Kulesza, M., Kane-Willis, K., Qin, S., & Smelson, D. (2017b). Developing a research agenda for understanding the stigma of addictions part II: Lessons from the mental health stigma literature. The American Journal on Addictiona, 26(1), 67-74. doi: 10.1111/ajad.12436
- Cummins, D. M., & Tobian, R. (2018). Motivational enhancement therapy for veterans with chronic pain and substance use. Health & Social Work, 43, 269 –273. http://dx.doi.org/10.1093/hsw/hly026
- da Silveira, P. S., Casela, A. L. M., Monteiro, E. P., Ferreira, G. C. L., de Freitas, J. V. T., Machado, N. M., Noto, A. R., & Ronzani, T. M. (2018). Psychosocial understanding of self-stigma among people who seek treatment for drug addiction. Stigma and Health, 3(1). 42-52. http://dx.doi.org/10.1037/sah0000069
- Dugosh, K., Abraham, A., Seymour, B., McLyd, K., Chalk, M., & Fstinger, D. (2016). A systematic review on the use of psychosocial interventions in conjunction with medications for the treatment of opioid addiction. Journal of Addictive Medicine, 10(2), 91-101. doi: 10.1097/ADM.0000000000000193
- Dydyk, A. M., Jain, N. K., & Gupta, M. (2020, June 22). Opioid use disorder. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK553166/
- Florence, C., Luo, F., & Rice, K. (2021). The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug and Alcohol Dependence, 218(1). https://doi.org/10.1016/j.drugalcdep.2020.108350
- Gatchel, R. J., McGeary, D. A., McGeary, C. A., & Lippe, B. (2014). Interdisciplinary chronic pain management. American Psychologist, 69(2), 119-130. doi: 10.1037/a0035514
- Goffman, E. (1963). Stigma: Notes on the management of spoiled identity [e-book edition]. Simon and Schuster. https://a.co/47eZuNE
- Hedegaard, H., Miniño, A. M., & Warner, M. (2020, January). Drug overdose deaths in the United States, 1999-2018. National Center for Health Statistics Data Brief, 356.
- Kelly, J. F., & Westerhoff, C. M. (2010). Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. The International Journal on Drug Policy, 21(3), 202–207. https://doi.org/10.1016/j.drugpo.2009.10.010
- Kelly, J. F., Wakeman, S. E., & Saitz, R. (2015). Stop talking ‘dirty’: Clinicians, language, and quality of care for the leading cause of preventable death in the United States. The American Journal of Medicine, 128(1), 8-9. https://www.amjmed.com/article/S0002-9343(14)00770-0/pdf
- Kennedy-Hendricks, A., Barry, C. L., Gollust, S. E., Ensminger, M. E., Chisolm, M. S., & McGinty, E. E. (2017). Social stigma toward persons with prescription opioid use disorder: Associations with public support for punitive and public health-oriented policies. Psychiatric Services, 68(5), 462–469. https://doi.org/10.1176/appi.ps.201600056
- Larimer, M. E., Palmer, R. S., & Marlatt, G. A. (1999). Relapse prevention. An overview of Marlatt’s cognitive-behavioral model. Alcohol Research & Health, 23, 151–160.
- Lee, E. B., An, W., Levin, M. E., & Twohig, M. P. (2015). An initial meta-analysis of acceptance and commitment therapy for treating substance use disorders. Drug & Alcohol Dependence, 155, 1–7. https://doi-org/10.1016/j.drugalcdep.2015.08.004
- Livingston, J. D., Milne, T., Fang, M. L., & Amari, E. (2012). The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. Addiction, 107(1), 39–50. https://doi.org/10.1111/j.1360-0443.2011.03601.x
- Luoma, J. B., Kulesza, M., Hayes, S. C., Kohlenberg, B., & Larimer, M. (2014). Stigma predicts residential treatment length for substance use disorder. The American Journal of Drug and Alcohol Abuse, 40(3), 206-212. https://doi.org/10.3109/00952990.2014.901337
- McGinty, E. E., & Barry, C. L. (2020). Stigma reduction to combat the addiction crisis – Developing an evidence base. The New England Journal of Medicine, 382(14), 1291-1292. doi: 10.1056/NEJMp2000227
- McGinty, E. E., Goldman, H. H., Pescosolido, B., & Barry, C. L. (2015). Portraying mental illness and drug addiction as treatable health conditions: Effects of a randomized experiment on stigma and discrimination. Social Science & Medicine, 126, 73-85. doi: http://dx.doi.org/10.1016/j.socscimed.2014.12.010
- McGinty, E., Pescosolido, B., Kennedy-Hendricks, A., & Barry, C. L. (2018). Communication strategies to counter stigma and improve mental illness and substance use disorder policy. Psychiatric Services, 69(2), 136-146. doi: 10.1176/appi.ps.201700076
- National Institute on Drug Abuse. (2018, January). Principles of drug addiction treatment: A research-based guide. Retrieved from https://www.drugabuse.gov/download/675/principles-drug-addiction-treatment-research-based-guide-third-edition.pdf?v=74dad603627bab89b93193918330c223
- O’Connell, M. J., Flanagan, E. H., Delphin-Rittmon, M. E., & Davidson, L. (2020). Enhancing outcomes for persons with co-occurring disorders through skills training and peer recovery support. Journal of Mental Health, 29(1), 6–11. https://doi-org/10.1080/09638237.2017.1294733
- Pollak, S. M., Pedulla, T., & Siegel, R. D. (2014). Three ways to bring mindfulness into therapy. Greater Good Science Center at UC Berkeley. Retrieved from https://greatergood.berkeley.edu/article/item/three_ways_bring_mindfulness_therapy
- Prochaska, J. O., & DiClemente, C. C. (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51, 390-395. http://dx.doi.org/10.1037/0022-006X.51.3.390
- Rohsenow, D. J., Monti, P. M., Martin, R. A., Colby, S. M., Myers, M. G., Gulliver, S. B., Brown, R. A., Mueller, T. I., Gordon, A., & Abrams, D. B. (2004). Motivational enhancement and coping skills training for cocaine abusers: Effects on substance use outcomes. Addiction, 99(7), 862–874. https://doi.org/10.1111/j.1360-0443.2004.00743.x
- Roos, C. R., Carroll, K. M., Nich, C., Frankforter, T., & Kiluk, B. D. (2020). Short- and long-term changes in substance-related coping as mediators of in-person and computerized CBT for alcohol and drug use disorders. Drug and Alcohol Dependence, 212. https://doi-org/10.1016/j.drugalcdep.2020.108044
- Saloner, B., McGinty, E. E., Beletsky, L., Bluthenthal, R., Beyrer, C., Botticelli, M., & Sherman, S. G. (2018). A public health strategy for the opioid crisis. Public Health Reports, 133I(I), 24S-34S. doi: 10.1177/0033354918793627
- Substance Abuse and Mental Health Services Administration [SAMHSA]. (n.d.). MAT medications, counseling, and related conditions. Retrieved from https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions
- Substance Abuse and Mental Health Services Administration [SAMHSA]. (2014, January). What is substance abuse treatment? A booklet for families. Retrieved from https://store.samhsa.gov/product/What-Is-Substance-Abuse-Treatment-A-Booklet-for-Families/SMA14-4126
- Substance Abuse and Mental Health Services Administration [SAMHSA]. (2020a, April 30). Mental health and substance use disorders. Retrieved from https://www.samhsa.gov/find-help/disorders
- Substance Abuse and Mental Health Services Administration [SAMHSA]. (2020b, April 23). Recovery and recovery support. Retrieved from https://www.samhsa.gov/find-help/recovery
- Tracy, K., & Wallace, S. P. (2016). Benefits of peer support groups in the treatment of addiction. Substance Abuse and Rehabilitation, 7, 143–154. https://doi.org/10.2147/SAR.S81535
- van Boekel, L. C., Brouwers, E. P. M., van Weeghel, J., & Garretsen, H. F. L. (2013) Stigma among health professionals towards patients with substance use disorders and its consequence for healthcare delivery: Systematic review. Drug and Alcohol Dependence, 131, 23-35. http://dx.doi.org/10.1016/j.drugalcdep.2013.02.018
- Yaugher, A.C., Atismé, K., Prestwick, H.u, Arrien, M.u , & Williams Condie, A. u (March, 2020).
- Reducing stigma toward medication-assisted treatment: An evidence-based overview of treatment of opioid use disorder
- [Fact Sheet]. Utah State University. Retrieved from https://extension.usu.edu/heart/research/reducingstigma
Authors
Chapel Taylor-Olsen, Hailey Judd, Ashley Yaugher, Rachel Myrer, Shane Bench
Related Research