Reducing Stigma Toward Medication-Assisted Treatment

This fact sheet serves to overview an essential evidence-based treatment for Opioid Use Disorder, Medication-Assisted Treatment. We also discuss the importance of reducing stigma when talking about treatment and recovery in this overview.
According to the Secretary of the U.S. Department of Health and Human Services, “a public health emergency exists nationwide as a result of the consequences of the opioid crisis.”
--Alex M. Azar II, April 15, 2019

Opioid Use Disorder (OUD) is a diagnosis given to an individual when opioid use causes significant distress or issues in their lives as a result of their use. A diagnosis of OUD includes building intolerance (i.e., needing a higher dose to have the same effect), withdrawal (i.e., illness caused by not having the substance), and/or misuse of an opioid (e.g., taken in larger amount than prescribed or longer than prescribed; American Psychiatric Association [APA], 2013).
Medication-Assisted Treatment (MAT)
MAT stands for Medication-Assisted Treatment. It uses a full-coverage approach by utilizing prescription medication in combination with counseling and behavioral therapies. There are substance use disorders that respond well to MAT. Opioid, alcohol, and nicotine addiction are all substance use disorders that can be treated with MATs (Bart, 2012; Sanger et al., 2018; Substance Abuse and Mental Health Services Administration [SAMHSA], 2018).
The focus in this brief review is Medication-Assisted Treatments based around OUD. There are three medications that can be used to treat OUD. These three medications are methadone or Dolophine®, buprenorphine or Subutex®, and naltrexone or Vivitrol® (Connery, 2015; Herbeck et al., 2008; McGovern & Carroll, 2003; SAMHSA, 2019b). Each of the medications described are prescribed based on individual needs in order to facilitate recovery (SAMHSA, 2019b). Medication-Assisted Treatments can also be particularly beneficial when prescribed in conjunction with behavioral therapy or counseling (Boisvert, et al., 2008; Carroll & Weiss, 2017; Dugosh, 2016; Evans, 2019).

“Medication-assisted treatment saves lives while increasing the chances a person will remain in treatment and learn the skills and build the networks necessary for long-term recovery.”
--Michael Botticelli, Director, National Drug Control Policy (2017).
The following table contains brief descriptions of each medication:
Methadone is an agonist medication that acts on opioid receptors in the brain by activating them. Methadone works to minimize withdrawal effects that occur when discontinuing or tapering the use of opioids (Fullerton et al. 2014; National Institute of Health [NIH], 2018; SAMHSA, 2019c). According to SAMSHA, methadone is best used when taken in a consistent dose over an extended length of time (i.e., 12 months or more; Moore, 2019). Methadone is safe if taken only as prescribed by a physician in a methadone treatment center (SAMHSA, 2019c).
Buprenorphine is a partial opioid agonist medication that acts on opioid receptors in the brain (SAMHSA, 2019a). It is more easily accessible than methadone because an individual can be prescribed buprenorphine in a standard health clinic rather than a methadone treatment center (Sokol et al., 2018; SAMHSA, 2019a). Similar to methadone, buprenorphine minimizes the withdrawal effects that come from discontinuing opioids (Fiellin, 2010; Haddad et al. 2014, NIH, 2018; SAMHSA, 2019a). Buprenorphine has a leveling-off effect that reduces dependency and misuse while providing less feelings of euphoria than a full agonist medication (SAMHSA, 2019a).
Naltrexone is completely different from methadone and buprenorphine because it is an opioid antagonist medication (Connery, 2015; Herbeck et al., 2008; McGovern & Carroll, 2003). This means that instead of mimicking the effects of an opioid, it blocks the effects altogether (SAMHSA, 2019d). While methadone and buprenorphine trick the brain into thinking it’s getting the desired opioids, naltrexone inhibits the brain from feeling intoxicated from opioids if they are used and lessens a person’s cravings to use opioids (SAMHSA, 2019d). It is important to note that individuals must be free from opioids for 7-10 days before their first dose of naltrexone (SAMHSA, 2019d).
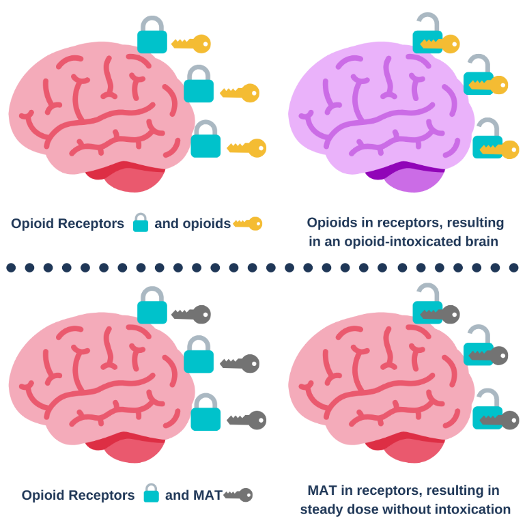
Figure 1
Figure 1 shows how opioids impact the brain (Pathan & Williams, 2012). Opioid receptors are the lock and opioids are the key that turn the receptor on, resulting in intoxication. Medication used for MAT fill the opioid receptors to help prevent opioid misuse and withdrawal symptoms (SAMHSA, 2019b). In other words, by using MAT, the individual does not have the same intoxicating effects which results in encouraging recovery.
Evidence Base for MAT
Despite the stigma, MAT is an evidence-based treatment.
MAT works well compared to other treatments:
- A long-term study following up on patients receiving MAT showed that after 18 months of treatment, less than 20% of patients were dependent on pain relievers, and after 48 months this dropped to less than 10% of patients (Julian, 2020; Potter et al., 2015).
MAT reduces overdose deaths:
- A study of 17,568 adults prescribed MAT showed that opioid overdose deaths decreased by 59% for those using Methadone and 38% for those prescribed buprenorphine (O’Malley, 2018; NIH, 2018).
Stigma
Stigma is a negative perception or attitude towards someone that devalues a person or group of people (Here to Help, 2014; Thornicroft, 2018). Stigma (avoiding someone, labeling them, or stereotyping) can result in a negative cycle leading to isolation, helplessness, and shame (Atisme, Arrington, Yaugher, & Savoie-Roskos, 2019). The following infographic, Figure 2, shows this negative cycle (National Academies of Sciences, Engineering and Medicine, 2016).
Stigma Towards OUD Treatment
What do we know? (Lefebvre et.al., 2019).
- A study of 997 participants showed just how stigmatized MAT and OUD are.
- One-third of participants believed that “medication-assisted-treatment. substitutes one addiction for another.”
- One-third refused to be seen by a physician that is treating patients with MAT to overcome their OUD.
- Around 40% of participants concluded that medications used in MAT are only “somewhat effective.”
- One-fourth believed that doctors should have the right to refuse treatment for individuals with OUD.

Figure 2
Stigma and Recovery
- It is important to remember that OUD can affect everyone differently. Additionally, treatment and recovery does not have one set way it should happen to be effective. It is based on the person’s preferences and what works for them, there is no single treatment that is the answer to all opioid use disorders (SAMHSA, 2019b).
- It is also important to remember that recovery is a journey, not a state of being. In most cases, recovery will not be a linear process, and that’s okay! Recovery is a lifelong process that the person will continue through in a way that is helpful to them (SAMHSA, 2019b).
- For more information, please check out our previous Stigma Fact Sheet: https://digitalcommons.usu.edu/extension_curall/1969/ (Atisme et al., 2019).
The information below shows actions you can take today to decrease stigma in your own life (Atisme, et al., 2019; Center for Motivation and Change, 2014; U.S. Department of Health and Human Services [HHS], 2004).
- Learn more about MAT and recovery by visiting some of the resources below.
- Encourage your loved one to get effective, evidence-based treatment
- Monitor your language.
- Seek counseling or advice for setting appropriate boundaries.
- Use positive reinforcement strategies instead of shaming or blaming.
- Seek to understand the person with a substance use disorder.

Actions to Reduce Stigma Related to MAT for OUD
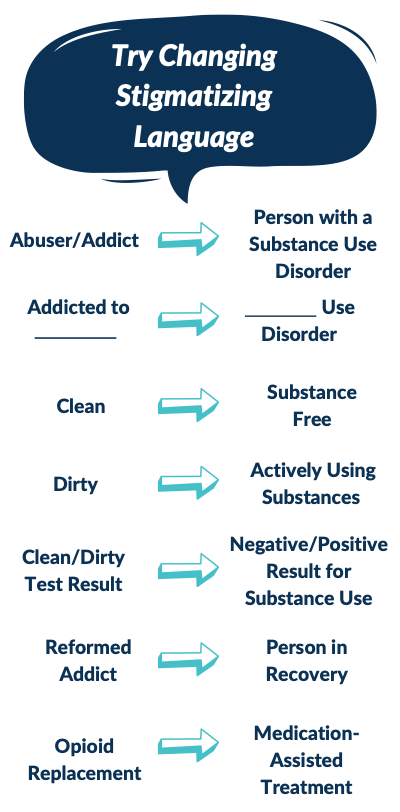
Figure 3
Figure 3 shows person-first language to help reduce stigma and open the conversation with a friend or loved one to encourage treatment and recovery (APA, n.d.; Botticelli & Koh, 2016; Kelly et al., 2015).
Websites
- The American Psychological Association (APA): http://www.apa.org/helpcenter/opioid-abuse.aspx
- Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/nchs/products/databriefs/db294.htm
- Mental Health America (MHA) Screenings: https://screening.mentalhealthamerica.net/screening-tools/
- National Alliance on Mental Illness (NAMI): http://www.nami.org/Find-Support/Living-with-a-Mental-Health-Condition/Taking-Care-of-Your-Body/Drugs,-Alcohol-Smoking
- National Institute on Drug Abuse (NIDA): https://www.drugabuse.gov/
- Substance Abuse and Mental Health Services Administration (SAMHSA): http://www.integration.samhsa.gov/clinical-practice/substance_use
- Substance Abuse and Mental Health Services Administration (SAMHSA) Find Treatment: https://findtreatment.samhsa.gov/
Books and Publications
- Bisaga, A., Chernyaev, K., McLellan, T. (2018). Overcoming Opioid Addiction: The Authoritative Medical Guide for Patients, Families, Doctors, and Therapists. The Experiment, 1st Edition, 2018.
- Substance Abuse and Mental Health Services Administration (2018). Medications for Opioid Use Disorder. Treatment Improvement Protocol (TIP) Series 63, Full Document. HHS Publication No. (SMA) 19-5063FULLDOC. Rockville, MD: Substance Abuse and Mental Health Services Administration. Retrieved from https://store.samhsa.gov/system/files/tip63_fulldoc_052919_508.pdf
- Effective Treatments for Opioid Addiction. National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services. Retrieved from https://d14rmgtrwzf5a.cloudfront.net/sites/default/files/policybrief-effectivetreatments.pdf
- Pain Management Best Practices Inter-Agency Task Force Report: Updates, Gaps, Inconsistencies, and Recommendations. Retrieved from: https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
- American Psychological Association. Guidelines for Bias-Free Language for Disability in APA journals (n.d.). Retrieved January 17, 2020 from https://apastyle.apa.org/style-grammar-guidelines/bias-free-language/disability
- Atisme, K.; Arrington, R.; Yaugher, A.; & Savoie-Roskos, M., "Substance Use Disorder Stigma: What It Is and How You Can Prevent It" (2019). All Current Publications. Paper 1969. https://digitalcommons.usu.edu/extension_curall/1969
- Azar, A. M. (2019, April 15). Renewal of Determination that a Public Health Emergency Exists. Retrieved January 16, 2020, from https://www.phe.gov/emergency/news/healthactions/phe/Pages/opioid-19apr2019.aspx
- Bart, G. (2012). Maintenance Medication for Opiate Addiction: The Foundation of Recovery. Journal of Addictive Diseases, 31(3), 207–225. doi: 10.1080/10550887.2012.694598
- Boisvert R.A., Martin L.M., Grosek M., Clarie A.J. (2008) Effectiveness of a peer-support community in addiction recovery: Participation as intervention. Occupational Therapy International, 15: 205-220
- Botticelli, M. P., & Koh, H. K. (2016). Changing the language of addiction. Jama, 316(13), 1361-1362.
- Botticelli, M. (2017). Remarks by ONDCP Director Michael Botticelli. Retrieved July 3, 2019, from https://obamawhitehouse.archives.gov/the-press-office/2015/09/17/remarks-ondcp-director-michael-botticelli
- Carroll K.M., Weiss R.D., (2017) The role of behavioral interventions in buprenorphine maintenance treatment: A review. The American Journal of Psychiatry, 174: 738-747 https://doi.org/10.1176/appi.ajp.2016.16070792
- Center for Motivation and Change [CMC]. (2014). What Is CRAFT. Retrieved July 16, 2019, from https://motivationandchange.com/outpatient-treatment/for-families/craft-overview/
- Connery, H. S. (2015). Medication-assisted treatment of opioid use disorder: review of the evidence and future directions. Harvard review of psychiatry, 23(2), 63-75.
- Dugosh, K., Abraham, A., Seymour, B., McLoyd, K., Chalk, M., &Festinger, D. (2016). A systematic review on the use of psychosocialinterventions in conjunction with medications for the treatment of opioidaddiction.Journal of Addiction Medicine, 10,93–103. doi: 10.1097/ADM.0000000000000193
- Fiellin, D.A., Moore, B.A., Sullivan, L.E., Becker, W.C., Pantalon, M.V., Chawarski, M.C., Schottenfeld, R.S., (2008) Long-term treatment with buprenorphine/naloxone in primary care: Results at 2–5 years. The American Journal on Addictions, 17: 116-120 https://doi.org/10.1080/10550490701860971
- Fullerton, C. A., Kim, M., Thomas, C. P., Lyman, D. R., Montejano, L. B., Dougherty, R. H., … Delphin-Rittmon, M. E. (2014). Medication-Assisted Treatment with Methadone: Assessing the Evidence. Psychiatric Services, 65(2), 146–157. doi: 10.1176/appi.ps.201300235
- Haddad, M.S., Zelenev, A., Altice, F.L. Buprenorphine maintenance treatment retention improves nationally recommended preventive primary care screenings when integrated into urban federally qualified health centers. Journal of urban health: bulletin of the New York Academy of Medicine, 92(1):193–213
- Herbeck, D.S., Hser, Y., Teruya, C. (2008). Empirically supported substance abuse treatment approaches: A survey of treatment providers’ perspectives and practices. AddictiveBehaviors,33 (5). 699-712. Doi: 10.1016/j.addbeh.2007.12.003
- Here to Help. (2014). Stigma and Discrimination Around Mental Health and Substance Use Problems. Retrieved July 2, 2019, from https://www.heretohelp.bc.ca/infosheet/stigma-and-discrimination-around-mental-health-and-substance-use-problems
- Julian, T. (2020). Long-Term Efficacy of Medication-Assisted Treatment of Opioid Addiction. Topics in Pain Management, 35(6), 1–9. doi: 10.1097/01.tpm.0000617884.40854.7f
- Kelly, J. F., Wakeman, S. E., & Saitz, R. (2015). Stop talking ‘dirty’: clinicians, language, and quality of care for the leading cause of preventable death in the United States. The American journal of medicine, 128(1), 8-9. https://www.amjmed.com/article/S0002-9343(14)00770-0/pdf
- Lefebvre, C., Squiers, L., Adams, E.T., Nyblade, L., West, S. & Bann, C. (2019). Stigma and prescription opioid addiction and treatment: A national survey. Society of Behavioral Medicine 40th Annual Meeting & Scientific Sessions. Download available at https://osf.io/uwhcn/
- McGovern, M. P., & Carroll, K. M. (2003). Evidence-based practices for substance use disorders. The Psychiatric clinics of North America, 26(4), 991–1010. https://doi.org/10.1016/s0193-953x(03)00073-x
- Medical Experts: Inadequate Federal Approach to Opioid Treatment and the Need to Expand Care, House Committee on Oversight and Reform (2019). (Testimony of Arthur C. Evans). Retrieved from https://docs.house.gov/meetings/GO/GO00/20190619/109654/HHRG-116-GO00-Wstate-EvansA-20190619.pdf
- Moore, K. E., Roberts, W., Reid, H. H., Smith, K. M., Oberleitner, L. M., & Mckee, S. A. (2019). Effectiveness of medication assisted treatment for opioid use in prison and jail settings: A meta-analysis and systematic review. Journal of Substance Abuse Treatment, 99, 32–43. doi: 10.1016/j.jsat.2018.12.003
- National Academies of Sciences, Engineering, and Medicine. (2016). Understanding Stigma of mental and substance use disorders. Ending discrimination against people with mental and substance use disorders: The evidence for stigma change (33-52). National Academies Press.
- National Institutes on Health [NIH]. (2018). Methadone and buprenorphine reduce risk of death after opioid overdose. Retrieved July 3, 2019, from https://www.nih.gov/news-events/news-releases/methadone-buprenorphine-reduce-risk-death-after-opioid-overdose
- O’Malley, P. (2019). Medication assisted therapy (MAT) for opioid use disorder (OUD) in youth improves outcomes and saves lives. Evidence Based Nursing. doi: 10.1136/ebnurs-2018-103053
- Pathan, H., & Williams, J. (2012). Basic opioid pharmacology: an update. British journal of pain, 6(1), 11-16.
- Potter, J. S., Dreifuss, J. A., Marino, E. N., Provost, S. E., Dodd, D. R., Rice, L. S., . . . Weiss, R. D. (2015). The multi-site prescription opioid addiction treatment study: 18-month outcomes. https://www.ncbi.nlm.nih.gov/pubmed/25189089
- Sanger, N., Shahid, H., Dennis, B. B., Hudson, J., Marsh, D., Sanger, S., … Samaan, Z. (2018). Identifying patient-important outcomes in medication-assisted treatment for opioid use disorder patients: a systematic review protocol. BMJ Open, 8(12). doi: 10.1136/bmjopen-2018-025059
- Sokol, R., Lavertu, A. E., Morrill, D., Albanese, C., & Schuman-Olivier, Z. (2018). Group-based treatment of opioid use disorder with buprenorphine: A systematic review. Journal of Substance Abuse Treatment, 84, 78–87. doi: 10.1016/j.jsat.2017.11.003
- Substance Abuse and Mental Health Services Administration [SAMHSA]. (2018). Medications for Opioid Use Disorder. Treatment Improvement Protocol (TIP) Series 63, Full Document. HHS Publication No. (SMA) 19-5063FULLDOC. Rockville, MD: Substance Abuse and Mental Health Services Administration. Retrieved from https://store.samhsa.gov/system/files/tip63_fulldoc_052919_508.pdf
- Substance Abuse and Mental Health Services Administration [SAMHSA]. (2019a). Buprenorphine. Retrieved July 12, 2019, from https://www.samhsa.gov/medication-assisted-treatment/treatment/buprenorphine.
- Substance abuse and Mental Health Services Administration [SAMHSA]. (2019b). Medication and Counseling Treatment. Retrieved July 10, 2019, from https://www.samhsa.gov/medication-assisted-treatment/treatment#medicaitons-used-in-mat.
- Substance Abuse and Mental Health Services Administration [SAMHSA]..(2019c). Methadone. Retrieved July 29, 2019, from https://www.samhsa.gov/medication-assisted-treatment/treatment/methadone.
- Substance Abuse and Mental Health Services Administration [SAMHSA]. (2019d). Naltrexone. Retrieved July 10, 2019, from https://www.samhsa.gov/medication-assisted-treatment/treatment/naltrexone
- Thornicroft, G., Rose, D., Kassam, A., & Sartorius, N. (2018). Stigma: Ignorance, prejudice or discrimination? Retrieved July 2, 2019, from https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/stigma-ignorance-prejudice-or-discrimination/E6F23CE48666A53C8E99870F0474E1AA/core-reader
- U.S. Department of Health and Human Services [HHS] Substance Abuse and Mental Health Services Administration’s [SAMHSA] Center for Substance Abuse Treatment [CSAT]. (2004). Substance Use Disorders: A Guide to the Use of Language. Retrieved from https://www.naabt.org/documents/Languageofaddictionmedicine.pdf
*Please note that all of the resources provided are for educational purposes and USU does not specifically endorse their services. These resources are intended to provide information, not to treat Opioid Use Disorder or other mental health concerns. USU does not control the websites or books referenced above.
In its programs and activities, Utah State University does not discriminate based on race, color, religion, sex, national origin, age, genetic information, sexual orientation or gender identity/expression, disability, status as a protected veteran, or any other status protected by University policy or local, state, or federal law. The following individuals have been designated to handle inquiries regarding non-discrimination policies: Executive Director of the Office of Equity, Alison Adams-Perlac, alison.adams-perlac@usu.edu, Title IX Coordinator, Hilary Renshaw, hilary.renshaw@usu.edu, Old Main Rm. 161, 435-797-1266. For further information on notice of non-discrimination: U.S. Department of Education, Office for Civil Rights, 303-844-5695, OCR.Denver@ed.gov. Issued in furtherance of Cooperative Extension work, acts of May 8 and June 30, 1914, in cooperation with the U.S. Department of Agriculture, Kenneth L. White, Vice President for Extension and Agriculture, Utah State University.
Authors
Ashley Yaugher, PhD; Kandice Atismè, MHA, MPH, CPH; Heidi Prestwich, Health & Wellness Intern; Melissa Arrien, Health & Wellness Intern; Alise Williams Condie, Health & Wellness Intern
Related Research








