Youth Treatment for a Substance Use Disorder and Common Barriers

This factsheet reviews youth substance use treatment, barriers that they face, prevention interventions, and resources for parents and community members.
Treatment Barriers
In the United States, a low proportion of adults with Opioid Use Disorder (OUD) who seek care actually receive treatment (Compton et al., 2019). This alarming trend is also evident in youth, where, of those who report seeking treatment for a Substance Use Disorder (SUD), only 35% report receiving treatment due to stigma, discrimination, insurance, wait list, and financial hardships (Robinson & Wilson, 2020). Along with structural and system barriers to adolescents receiving treatment for a SUD (e.g., parental consent required for youth under 18 in most states), the societal barrier of stigma contributes to adolescents not receiving care for their SUD (Alinsky et al., 2020). Additionally, adolescent-serving treatment programs have been shown to be half as likely than adult-serving programs to provide evidence-based, Medication Assisted Treatment to their patients (Alinsky et al., 2020).
See Figure 1 below, for data on Utah youth treatment need compared to those who received treatment.
Figure 1.
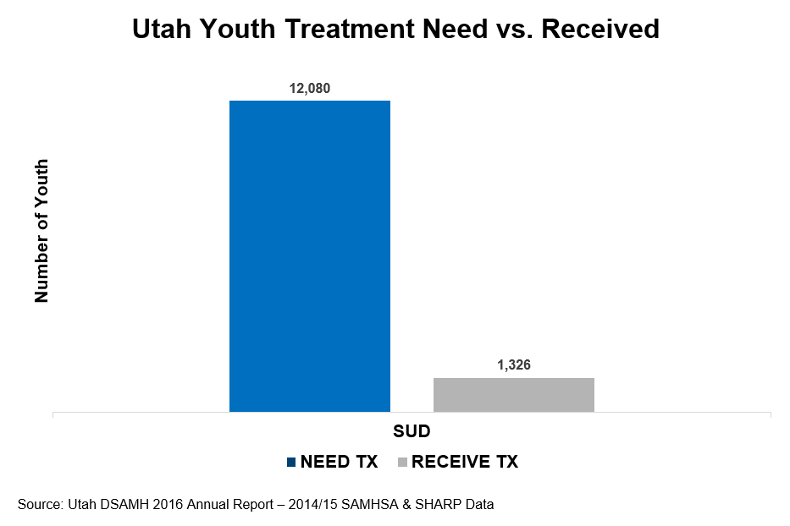
Source: Burrow-Sánchez, J. (2019, June 19). Understanding the Social and Biological Aspects of Adolescent Development: The Implications for Substance Use Prevention. https://utahprevention.org/wp-content/uploads/2019/08/burrow_sanchez_bryce.pdf.
Intervention Barriers
An intervention is an action or program carried out by medical professionals, public health professionals, and coalitions and community members. Interventions are focused on improving various aspects of health through prevention, policy, or other means (Minnesota Department of Health, 2001). Interventions aimed as a “one-size-fits-all” approach often do not meet all of the needs of each person in a community. For example, interventions that target the public do not fit the unique needs of youth in foster care (Braciszewski et al., 2014). Breaking off newly formed relationships with individuals providing interventions can be harmful to these youth because of issues associated with transient relationships. Effective interventions for this population should be engaging and use a variety of preventions and treatment efforts (Braciszewski et al., 2014). If you feel that the intervention currently being used for your young person has not been effective, talk with your primary care provider about other options as some interventions are not right for everyone (Braciszewski et al., 2014).
Preventing a Substance Use Disorder
Some of the responses aimed at addressing the U.S. opioid crisis include interventions, policies, and practices (see Figure 2 below) that can increase protection and decrease the risk of children and adolescents developing a SUD (Compton et al., 2019). Substance use prevention efforts including treatment, overdose prevention, and recovery support services, should be included in overall health efforts for youth (De Nadia, et al., 2019).
Adverse Childhood Experiences (ACEs) can cause an extensive effect on substance use in adolescence and across the lifespan (Stein, et al., 2017). Primary prevention interventions focused on reducing ACEs could reduce the likelihood of a youth developing a SUD (Compton et al., 2019). Examples of primary prevention interventions from the CDC aimed at reducing ACEs include:
- Strengthening economic supports to families
- Changing social norms to support parents and positive parenting
- Providing quality care and education early in life
- Enhancing parenting skills to promote healthy child development
- Intervening to lessen harms and prevent future risk (Adverse Childhood Experiences [ACEs], 2020).
For lasting change, long-term intervention approaches such as society-wide distribution of treatment resources, program designs for specific treatment centers, and personalized care for youth are extremely effective and essential (De Nadai et al., 2019). Community coalitions and parents can be involved in this type of change. See Figure 2 below for interventions, policies, and practices that can be applied to your family or community.
Figure 2.
| Interventions | Policies | Practices |
|---|---|---|
| Rescue interventions aimed at saving a life from overdose (e.g., naloxone and harm reduction trainings) | Restrictions to the initial fill of short-acting opiates to no more than a 7-day supply and a 3-day supply for prescriptions from a dentist (Factsheet: Utah’s Oversight of Opioid Prescribing and Monitoring of Opioid Use, 2019). | Support evidence-based recoveries including Medication Assisted Treatment. |
Primary prevention is aimed at preventing substance use disorder before it ever occurs (Kisling & Das, 2020)
|
Health insurers may facilitate non-narcotic treatment alternatives for patients with chronic pain and Medication Assisted Treatment for patients with opioid dependence disorder (Factsheet: Utah’s Oversight of Opioid Prescribing and Monitoring of Opioid Use, 2019). | Create safe spaces for people to be seen and heard. |
| Prescribers must check the controlled substance database before issuing the first prescription of an opioid to a patient unless the prescription is for 3 days or less or for a 30-day post-surgery supply (Factsheet: Utah’s Oversight of Opioid Prescribing and Monitoring of Opioid Use, 2019). | Improve prescribing practices through provider education and training. | |
| A person who reports an overdose may claim an affirmative defense to specified charges of violating the Utah Controlled Substances Act if they remain and cooperates with EMS and law enforcement (Factsheet: Utah’s Oversight of Opioid Prescribing and Monitoring of Opioid Use, 2019). | Halt the supply of illicit opioids through securing the borders and strengthening criminal penalties for drug traffickers. | |
| Try alternative methods to prescription opioids (e.g., mindfulness, meditation, yoga, or nonprescription pain medications). | ||
| Practice safe storage by locking opioids out of reach from children, pets, and guests, know how many pills should be in the bottle, and store opioids in the original bottle. For more information, visit useonlyasdirected.org/opioid-safety/ | ||
| Dispose of opioids safely by using a pharmacy’s or law enforcement agency’s medication drop box or by home disposal through mixing medications with kitty litter, a soiled diaper, or used coffee grounds in a sealed bag. For more information, visit useonlyasdirected.org/throw-out/ |
What you can do to Help with Youth Substance Use Disorder Interventions
In Figure 2 above there are examples of interventions including overdose rescue and primary prevention, policies, and practices to reduce and treat substance use disorder in youth. Below is a list of parent and community resources that can be helpful in this work. Consider partnering with your local prevention professionals for additional resources and support to positively impact our youth’s futures.
Parent and Community Resources
| Organization | Website |
|---|---|
|
Al-Anon/Alateen |
|
|
Communities That Care |
|
|
CRAFT Family Support |
|
|
Naloxone |
naloxone.utah.gov/ |
|
National Harm Reduction Coalition |
harmreduction.org/ |
|
National Substance Use Treatment Locator |
findtreatment.gov/ |
|
National Suicide Prevention Lifeline (1-800-723-8255) |
suicidepreventionlifeline.org/ |
| Parents Empowered | parentsempowered.org/ |
| SafeUT | safeut.med.utah.edu/ |
| SMART Recovery | myusara.com/smart-recovery-at-usara/ |
| Substance Abuse Mental Health Services Administration (SAMHSA) | samhsa.gov |
| The Opidemic | |
| United Way (2-1-1) | 211utah.org/ |
| Use Only as Directed | useonlyasdirected.org/ |
| USU Health Extension: Advocacy, Research Teaching (HEART) Initiative | extension.usu.edu/heart/ |
| Utah Coalitions for Opioid Overdose Prevention | ucoop.utah.gov/ |
| Utah Department of Human Services, Substance Abuse and Mental Health | dsamh.utah.gov/ |
| Utah Poison Control Center
(1-800-222-1222) |
poisoncontrol.utah.edu/ |
| Utah Prevention Coalition Association | utahprevention.org/ |
| Utah Support Advocates for Recovery Awareness | myusara.com/ |
References
- Alinsky, R. H., Hadland, S. E., Matson, P. A., Cerda, M., & Saloner, B. (Accepted/In press). Adolescent-Serving Addiction Treatment Facilities in the United States and the Availability of Medications for Opioid Use Disorder. Journal of Adolescent Health. https://doi.org/10.1016/j.jadohealth.2020.03.005
- Braciszewski, J. M., Moore, R. S., & Stout, R. L. (2014). Rationale for a New Direction in Foster Youth Substance Use Disorder Prevention. Journal of substance use, 19(1-2), 108–111. https://doi.org/10.3109/14659891.2012.750693
- Burrow-Sánchez, J. (2019, June 19). Understanding the Social and Biological Aspects of Adolescent Development: The Implications for Substance Use Prevention. https://utahprevention.org/wp-content/uploads/2019/08/burrow_sanchez_bryce.pdf.
- Centers for Disease Control and Prevention. (2020, April 3). Adverse Childhood Experiences (ACEs). Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/acestudy/.
- Compton, W. M., Jones, C. M., Baldwin, G. T., Harding, F. M., Blanco, C., & Wargo, E. M. (2019). Targeting Youth to Prevent Later Substance Use Disorder: An Underutilized Response to the US Opioid Crisis. American Journal of Public Health, 109, S185–S189. https://doi-org.dist.lib.usu.edu/10.2105/AJPH.2019.305020
- De Nadai, A. S., Little, T. B., McCabe, S. E., & Schepis, T. S. (2019). Diverse Diagnostic Profiles Associated With Prescription Opioid Use Disorder in a Nationwide Sample: One Crisis, Multiple Needs. Journal of Consulting & Clinical Psychology, 87(10), 849–858. https://doi-org.dist.lib.usu.edu/10.1037/ccp0000429
- Factsheet: Utah’s Oversight of Opioid Prescribing and Monitoring of Opioid Use. (2019, February). https://oig.hhs.gov/oas/reports/region7/71805115_Factsheet.pdf.
- Kisling L. & Das J. (2020, Jun 7). Prevention Strategies. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537222/
- Minnesota Department of Health. (2001). Public health interventions: Applications for public health nursing practice.
- Robinson, C. A., & Wilson, J. D. (2020). Management of Opioid Misuse and Opioid Use Disorders Among Youth. Pediatrics, 145, S153–S164. https://doi-org.dist.lib.usu.edu/10.1542/peds.2019-2056C
- Stein, M. D., Conti, M. T., Kenney, S., Anderson, B. J., Flori, J. N., Risi, M. M., & Bailey, G. L. (2017). Adverse childhood experience effects on opioid use initiation, injection drug use, and overdose among persons with opioid use disorder. Drug & Alcohol Dependence, 179, 325–329. https://doi-org.dist.lib.usu.edu/10.1016/j.drugalcdep.2017.07.007
* In its programs and activities, Utah State University does not discriminate based on race, color, religion, sex, national origin, age, genetic information, sexual orientation or gender identity/expression, disability, status as a protected veteran, or any other status protected by University policy or local, state, or federal law. The following individuals have been designated to handle inquiries regarding non-discrimination policies: Executive Director of the Office of Equity, Alison Adams-Perlac, alison.adams-perlac@usu.edu, Title IX Coordinator, Hilary Renshaw, hilary.renshaw@usu.edu, Old Main Rm. 161, 435-797-1266. For further information on notice of non-discrimination: U.S. Department of Education, Office for Civil Rights, 303-844-5695, OCR.Denver@ed.gov. Issued in furtherance of Cooperative Extension work, acts of May 8 and June 30, 1914, in cooperation with the U.S. Department of Agriculture, Kenneth L. White, Vice President for Extension and Agriculture, Utah State University.
Authors
Kandice Atismé; Jaclyn Atencio Miller, Health & Wellness Intern
Related Research






