Community Paramedicine: A New Approach to Health in Rural Communities

What is Community Paramedicine?
The community paramedicine (CP) concept is becoming widely used in rural communities to assist in maintaining and improving health across economic and geographic disparities. This model utilizes highly trained emergency medical service (EMS) professionals under the supervision of a physician or other advanced practice practitioner (i.e., physician assistants and advanced practice registered nurses; Patterson et al., 2016) to provide a variety of needed health services tailored to community needs. CP has been shown to be effective in many communities and, given these positive results, should be considered in rural communities where geographic barriers limit access to healthcare (Martin & O'Meara, 2019). This fact sheet will review the positive impacts that CP can have in a community, the policy required to start CP, and how individuals can advocate for CP in their community.
How Community Paramedicine Can Help
CP with EMS providers can serve many issues and provide preventative care or aftercare as well as testing for health conditions (Patterson et al., 2016). While the broad concept is the same in using the skills of accessible EMS professionals, each community uses CP in a different way to meet the health needs of the area
(Figure 1). Some programs assist with the maintenance of chronic diseases and offer in-home primary care services utilizing CP practitioners (Nolan et al., 2018). Other programs focus on improving post-hospitalization outcomes and use CP practitioners to provide scheduled, post-discharge follow-ups with patients (Patterson et al., 2016).

Many people, especially older adults, find that aftercare is difficult after receiving care at the hospital or an emergency department (ED) (Shah et al., 2018). CP is equipped to provide around-the-clock care that is always accessible as part of the community's existing emergency services. Further, CP builds a bond of trust when paramedicine providers offer health coaching
(Nejtek et al., 2017).
CP paramedics help with the follow-up care that is personalized and includes a medical education component, which improves patient satisfaction and health (Cameron & Carter, 2019; Nolan et al., 2018; Shah et al., 2018).
In types of medical issues that carry stigma (e.g., infectious disease, substance use, mental health issues, etc.), having a trusted CP offering in-home services can lead to early intervention and better care.
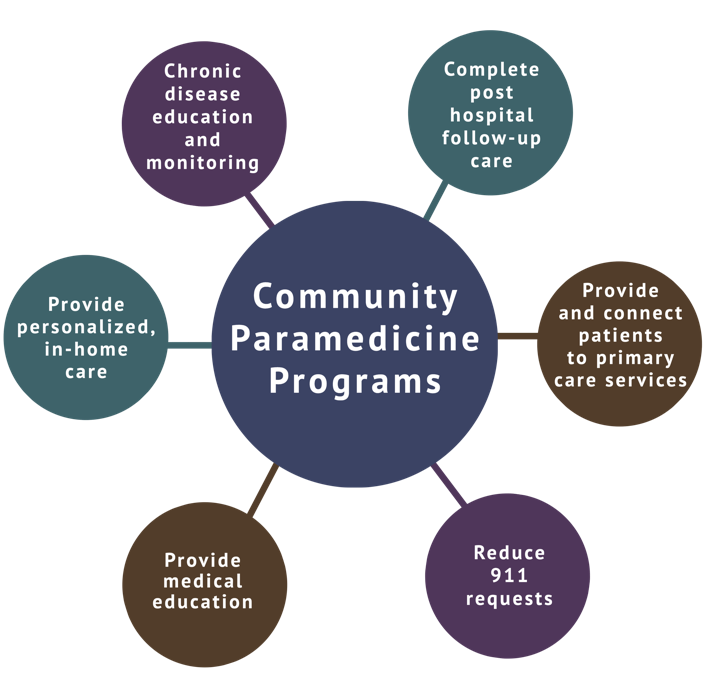
Figure 1. Uses of Community Paramedicine Programs
CP is promising for reducing healthcare costs as well as improving access to services (Patterson et al., 2016). Specifically, by addressing the education of patients on various topics (e.g., managing chronic conditions, mental health, aftercare, etc.), improving access to health monitoring, and improving supports for vulnerable populations, CP can fill a gap in health services (Martin & O'Meara, 2019). The use of CP for mobile integrated health services can improve quality of life, reduce pain, and improve mobility (Gregg et al., 2019; Nejtek et al., 2017). Additionally, this model improves patient satisfaction with their health care needs (Gregg et al., 2019).
There are many barriers in rural areas that lead to lack of services, and one way to help with this is increased public health services along with training professionals to implement more comprehensive services (Johansson et al., 2019). CP is essential for many rural communities that do not have access to critical healthcare resources and is expanding with more home care partnerships and wellness clinics (Cameron & Carter, 2019). CP can benefit rural communities and EMS agencies by:
- "Reducing 9-1-1 requests for non-urgent, non-transport services that are not reimbursable.
- Decreasing the 'downtime' between calls, exercising medical skills, and improving access to providers to meet the community's primary care needs.
- Increasing revenue by billing patients or third-party payers for services provided, when appropriate" (Rural Health Information Hub, n. d.).
- Reducing paramedic service utilization and hospital attendance and improving health outcomes.
- Significantly increasing health care cost savings (Martin & O'Meara, 2019).
How Community Paramedicine Works
The Joint Committee on Rural Emergency Care (JCREC) defines a CP paramedic as someone who:
- Holds a state-license as an EMS professional.
- Completes an appropriate education program.
- Demonstrates competence in the provision of health education, monitoring, and services.
- Monitors chronic disease and educates patients.(Rural Health Information Hub, n.d., para. 4)
The general paramedicine curriculum from the National Association of Emergency Medical Technicians (n.d.) operates under the supervision of a physician or advanced practice provider and is conducted by a paramedic or EMS care provider that has extensive training. It includes the following EMS training and skills:
- Assessing patients.
- Initiating life-sustaining stabilization.
- Treating acute or chronic illness and/or injuries.
- Transporting to an ED.
- Releasing to a higher level of care.
- Performing all trained skills, including:
- Advanced airway management (such as endotracheal intubation).
- Electrocardiographs (ECGs).
- Inserting intravenous (IV) lines.
- Administering numerous emergency medications.
- Assessing ECG tracings.
- Defibrillation.
Beyond the skills listed above, the additional clinical educational requirements under the CP model include training in preparing and following an existing collaborative medical care plan for a patient's health care services outside of the hospital.
Goals of Community Paramedicine
Goals of the CP Model
- Prevent hospitals readmission.
- Identify and support frequent EMS and ED users.
- Manage multiple chronic conditions (such as congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), asthma, and diabetes.
- Evaluate and manage chronic disease.
- Assess and stabilize patients with a behavioral health diagnosis.
- Determine alternative destinations (including clinics and doctors’ offices, with appropriate regional EMS scope of practice permission).
- Improve the patient's quality of life.
- Decrease overall healthcare costs.
CP activities must be allowable/supportable within EMS regulations, licensure, certification, and scope of practice for the regions and providers utilizing the model. The use of CP is intended to expand providers’ reach in primary care and the public health service. The specific rules and services are determined by community health needs and in collaboration with public health and medical direction.
Successful Examples of Community Paramedicine
- California – Commonwealth Care Alliance. In recent years, the practice of CP has become increasingly utilized with significant successes. Hegwer (2019) showed that Commonwealth Care Alliance, a healthcare company in California, reduced unnecessary ED visits and hospitalizations by using CP and specially trained paramedics in targeted California communities. By assessing and stabilizing at-risk patients at home under a physician's supervision instead of the hospital, CP prevented unnecessary transports, ED visits, and hospitalizations. This change generated savings of approximately $1,900 per case, with a total cost savings of approximately $6 million over one year
(Hegwer, 2019). - Maine. Maine's population is older than many states, with 18% of the state aged 65 years or older. Maine's population is also considered rural, with higher poverty rates and lower incomes. CP was used in Maine to address these issues by providing episodes of patient evaluation, advice, and treatment to prevent or improve medical conditions within their scope of practice, under the direction of a doctor. CP providers performed blood draws, medication reconciliation, diabetes care, in-home fall prevention assessments, wound care, and more (Pearson & Shaler, 2017).
- California – HOME Team. In California, the Homeless Outreach and Medical Emergency
(HOME) Team CP program was developed to find frequent emergency service users, connect them to community-based care, and advocate for long-term care when appropriate. The HOME Team provided care to 59 individuals who had used emergency services four or more times per month during the last 15 months. Approximately one-third were homeless, and the majority of individuals cared for had a substance use disorder at the time of contact and had a history of psychiatric disorder. The clinical planning resulted in new, long-term care placement options for patients with both mental health and substance use disorders (Kizer et al., 2013; Rasku et al., 2019). - Pennsylvania, Minnesota, and Colorado. Organizations like Geisinger in Danville, Pennsylvania and North Memorial Health Care in Robbinsdale, Minnesota are using specially trained paramedics to assess and stabilize at-risk patients, thus avoiding unnecessary ED visits and hospitalizations. Colorado CP programs were used to address the gap between EMS and health care as a way to cut down on lengthy home health needs and for home-based primary care ordered by doctors for chronic disease monitoring and educational services (Martin & O'Meara, 2019). In total, 48 states report supporting the CP model of care (National Association of State EMS Officials, 2020). With savings of up to $8,500 per patient reported in a study of reduced inpatient ED usage (Ahlers et al., 2018), CP is a value in health care that cannot be ignored.
- Canada. In a rural community in Canada, where community paramedicine has become more prevalent, a qualitative study showed a significant desire to increase education to provide these essential services (e.g., chronic disease management, crisis intervention, care for aging populations, and health education) as integral components of implementing this model (O'Meara et al., 2014).
Payment Paradigms and Policy Considerations
The use of EMS providers outside of the traditional prehospital care emergency response "load and go" format is not a new paradigm. Communities have been relying on licensed/certified paramedics and EMTs for many years to provide hospital emergency coverage in the event of staffing shortages and catastrophic emergencies. The progression in using EMS providers outside of their original scope of practice and into CP and other nontraditional fields occurred in areas with fewer traditional medical providers (e.g., MDs, DOs, NPs, PAs, etc.), noncompliant patients, and high costs
(Rural Health Information Hub, n.d.). While EMS is used in these circumstances, the difficulty has been in qualifying for reimbursement and payment for these nontraditional services.
The ability of states to be reimbursed for care by Medicaid is an essential part of the CP equation. In 2013, the Centers for Medicare and Medicaid Services (CMS) changed the rule about who could be reimbursed through Medicaid for delivering preventive services. This change allows services by a CP provider to be covered as long as a physician or other licensed practitioner recommends those services (CMS, 2013). Some states have passed legislation to allow for reimbursement from Medicaid (Bennett et al., 2018), and some private insurance companies have agreed to reimburse for programs (Rural Health Information Hub, n.d.).
Examples of cost savings and community benefit from CP include (Hegwer, 2019):
- Improving responsiveness to people with mental illness.
- Reducing 30-day readmission inpatient rates.
- Improving patients' medication and dietary prescribed treatment adherence.
- Reducing EMS transports for frequent users.
- Providing accelerated patient referrals to Social Services.
- Improving compliance in patients with tuberculosis (TB).
- Reducing risks to themselves and the community.
- Reducing the incidence of unwanted transport of patients in hospice.
Because CP is a new concept, implementing programs can be difficult because of the lack of rules, regulations, and laws defining the programs. According to an analysis in 2017, all 50 states have laws for governing emergency medical systems, while 16 states have laws pertaining to CP, and concluded that there was a lack of guidance and consistency for CP programs and their scopes of practice (Glenn et al., 2018). Currently, Utah does not have enabling legislation or education requirements for CP. A community gap assessment has not been completed for the state, making it difficult to determine if CP programs will benefit Utah communities.
Some challenges of implementing CP include (Flex Monitoring Team, 2014):
- Potential overlap with other healthcare and home healthcare professionals.
- Issues of recruitment, retention, and medical direction.
- Geographic barriers.
- Inadequate opportunities along with limited financial resources for training.
- Issues of licensure, scope of practice, integration, and reimbursement.

For Utah to have a successful and sustainable CP program, it needs to complete a gap assessment and establish important parameters to determine spread within the scope of practice and training requirements.
Conclusion
The evidence from multiple communities suggests a great deal of value in a CP model, which can offer follow-up care, chronic disease management, in-home services, patient education, and more. Barriers to reimbursement rates and policy considerations can be addressed, but only if the community’s citizens recognize the need for a CP model and advocate for better access to care. In Utah, the benefits of using EMS services in geographically dispersed areas to offer better access to healthcare is a massive advantage of CP implementation. By using CP and bringing community partners and coalitions together, CP can be adapted to fill the healthcare needs and overcome the barriers in rural communities.
References
- Ahlers, M., Kershaw, J., & Wilcox, M. (2018, September). Community paramedic education drives evidence-based practice and health care cost savings. Poster presented at the meeting of Emergency Nursing 2018, Pittsburg, PA. https://sigma.nursingrepository.org/handle/10755/16565
- Bennett, K. J., Yuen, M. W., & Merrell, M. A. (2018). Community paramedicine applied in a rural community. Journal of Rural Health, 34(Suppl 1), s39–s47. https://doi.org/10.1111/jrh.12233
- Cameron, P., & Carter, A. (2019). Community paramedicine: A patch, or a real system improvement? Canadian Journal of Emergency Medicine, 21(6), 691–693. https://doi.org/10.1017/cem.2019.439
- Center for Medicaid and CHIP Services [CMS]. (2013). Update on preventive services initiatives. Department of Health and Human Services. https://www.medicaid.gov/Federal-Policy-Guidance/Downloads/CIB-11-27-2013-Prevention.pdf
- Flex Monitoring Team (2014). The evidence for community paramedicine in rural areas: State and local findings and the role of the state flex program. Flex Monitoring Team – University of Minnesota, University of North Carolina at Chapel Hill, University of Southern Maine. http://www.flexmonitoring.org/wp-content/uploads/2014/03/bp34.pdf
- Glenn, M., Zoph, O., Weidenaar, K., Barraza, L., Greco, W., Jenkins, K., Paode, P., & Fisher, J. (2018). State regulation of community paramedicine programs: A national analysis. Prehospital Emergency Care, 22(2), 244–251. https://doi.org/10.1080/10903127.2017.1371260
- Gregg, A., Tutek, J., Leatherwood, M. D., Crawford, W., Friend, R., Crowther, M., & McKinney, R. (2019). Systematic review of community paramedicine and EMS mobile integrated health care interventions in the United States. Population Health Management, 22(3), 213–222. https://doi.org/10.1089/pop.2018.0114
- Hegwer, L. R. (2019, February 18). Community paramedicine saves organization $6M in 1 year. Healthcare Financial Management Association. Retrieved June 15, 2020, from https://www.hfma.org/topics/article/63296.html
- Johansson, P., Blankenau, J., Tutsch, S. F., Brueggemann, G., Afrank, C., Lyden, E., & Khan, B. (2019). Barriers and solutions to providing mental health services in rural Nebraska. Journal of Rural Mental Health, 43(2-3), 103-107. https://doi.org/10.1037/rmh0000105
- Kizer, K. W., Shore, K., & Moulin, A. (2013). Community paramedicine: A promising model for integrating emergency and primary care. University of California - Davis. https://escholarship.org/uc/item/8jq9c187
- Martin, A. C., & O'Meara, P. (2019). Perspectives from the frontline of two North American community paramedicine programs: An observational, ethnographic study. Rural and Remote Health, 19(1), 4888. https://doi.org/10.22605/RRH4888
- National Association of Emergency Medical Technicians (NAEMT). (n.d.). Emergency medical technician-basic: National standard curriculum.
https://www.ems.gov/pdf/education/Emergency-Medical-Technician/EMT_Basic_1996.pdf - National Association of State EMS Officials. (2020, May 27). 2020 National emergency medical services assessment. https://www.ems.gov/pdf/2020_National_EMS_Assessment.pdf
- Nejtek, V. A., Aryal, S., Talari, D., Wang, H., & O'Neill, L. (2017). A pilot mobile integrated healthcare program for frequent utilizers of emergency department services. American Journal of Emergency Medicine, 35(11), 1702–1705. https://doi.org/10.1016/j.ajem.2017.04.061
- Nolan, M. J., Nolan, K. E., & Sinha, S. K. (2018). Community paramedicine is growing in impact and potential. Canadian Medical Association Journal, 190(21), E636-E637. https://doi.org/10.1503/cmaj.180642
- O'Meara, P., Ruest, M., & Stirling, C. (2014). Community paramedicine: Higher education as an enabling factor. Australasian Journal of Paramedicine, 11(2). https://doi.org/10.33151/ajp.11.2.22
- Patterson, D. G., Coulthard, C., Garberson, L. A., Wingrove, G., & Larson, E. H. (2016). What is the potential of community paramedicine to fill rural health care gaps? Journal of Health Care for the Poor and Underserved, 27(4A), 144–158. https://doi.org/10.1353/hpu.2016.0192
- Pearson K. B. & Shaler, G. (2017). Community paramedicine pilot programs: Lessons from Maine. Journal of Health and Human Services Administration, 40(2), 141–185. https://digitalcommons.usm.maine.edu/ems/4/
- Rasku, T., Kaunonen, M., Thyer, E., Paavilainen, E., & Joronen, K. (2019). The core components of community paramedicine–integrated care in primary care setting: A scoping review. Scandinavian Journal of Caring Sciences, 33(3), 508–521. https://doi.org/10.1111/scs.12659
- Raven, M. C., Kushel, M., Ko, M. J., Penko, J., & Bindman, A. B. (2016). The effectiveness of emergency department visit reduction programs: A systematic review. Annals of Emergency Medicine, 68(4), 467–483.
https://doi.org/10.1016/j.annemergmed.2016.04.015 - Rural Health Information Hub (n.d.). Community paramedicine. Retrieved June 19, 2020, from
https://www.ruralhealthinfo.org/topics/community-paramedicine - Shah, M. N., Hollander, M. M., Jones, C. M., Caprio, T. V., Conwell, Y., Cushman, J. T., DuGoff, E. H., Kind, A., Lohmeier, M., Mi, R., & Coleman, E. A. (2018). Improving the ED-to-home transition: The community paramedic-delivered care transitions intervention-preliminary findings. Journal of the American Geriatrics Society, 66(11), 2213–2220. https://doi.org/10.1111/jgs.15475
Authors
Kandice Atismé, Kira Swensen, Maren Voss, Hailey Judd, Emma Parkhurst, Ashley Yaugher, Timothy Keady
Related Research















