Equine Navicular Syndrome

Introduction
Equine navicular syndrome greatly affects the horse industry by accounting for up to one-third of all chronic forelimb lamenesses.1 While the exact cause and development of this disease are still widely controversial, there are noticeable and significant changes to the internal anatomy and structures that could contribute to the possible onset of lameness.
Three main causes are proposed that could play a role in the progression of this syndrome: biomechanical forces, vascular alterations, and chronic inflammation. The clinical signs of navicular syndrome can range from short, choppy strides to intermittent lameness, as well as gait changes and pain associated with the frog and heel.2 There are several options for diagnosing navicular syndrome, and many routes for treatment. While navicular syndrome is not curable, efforts can be made to slow the progression of navicular degeneration and reduce discomfort in the horse.
Causes of Navicular Syndrome

A – Third metacarpal (cannon) bone
B – Proximal phalanx (long pastern) bone
C – Middle phalanx (short pastern) bone
D – Distal phalanx (coffin) bone
E – Distal sesamoid (navicular) bone
F – Deep digital flexor tendon (DDFT)
The hoof contains a small bone called the distal sesamoid (navicular bone), located behind the short pastern bone and coffin bone joint (Figure 1).
The primary function of the navicular bone is to provide a constant angle of insertion for the deep digital flexor tendon (DDFT).1 Considerable forces are applied to the navicular bone when the foot is weight-bearing, which can cause degeneration of the structures over time and therefore create pain and lameness that can be classified as navicular syndrome. Other biomechanical factors that can contribute to this syndrome include large body size, improper shoeing, trimming and hoof conformation, as well as excessive intense training.3
It has also been proposed that vascular changes in the hoof could cause navicular syndrome. Decreased blood supply to the hoof can lead to pain and necrosis of the bone. Narrow hooves with tall heels were found to block adequate blood flow to the digital vessels, increasing the risk of degeneration.4 Other studies found that hyperemia (increased vascularity) could also cause symptoms of navicular syndrome. Lastly, chronic inflammation is considered to play a role in the onset of this syndrome.
Most theorize that navicular syndrome closely resembles osteoarthritis, where prolonged periods of inflammation result in damage to the surrounding structures. Changes in the fibrocartilage, surface fraying of the deep digital flexor tendon, as well as lesions and adhesions all suggest that navicular syndrome involves “abnormal loads applied to normal structures or normal loads applied to abnormal structures” resulting in the breakdown of function in this region of the hoof.1 These documented changes of the navicular bone and surrounding tissue suggest possible origins of the disease, with most cases involving a combination of the three suggested causes. However, further study is needed to understand the true cause of navicular syndrome better.
Clinical Signs and Diagnosing Navicular Syndrome

A – Third metacarpal (cannon) bone
B – Proximal phalanx (long pastern) bone
C – Middle phalanx (short pastern) bone
D – Distal phalanx (coffin) bone
E – Distal sesamoid (navicular) bone
Diagnosis of navicular syndrome depends on each case’s history and clinical signs. Most horses show signs of inconsistent performance, gait changes, loss of suppleness, and chronic intermittent lameness. A short choppy stride, especially if worked in a tight circle or on a hard surface, can also indicate this syndrome.2 Evaluating clinical lameness can be done by quantitative gait analysis using force plates that measure the amount of force when each limb strikes the plate. This can objectively show the degree of lameness in each limb.3
Another way to identify lameness in a particular limb is by doing a flex test on each leg and then analyzing their gait as they trot away. Flexing the limb for a set amount of time applies force to each joint while the veterinarian then watches to see how long it takes the horse to recover when they move out. A lameness score can then be assigned depending on their reaction. Hoof testers are also a great tool to help locate a specific region of pain in the hoof. Some navicular cases will show sensitivity and pain in the caudal heel and frog.
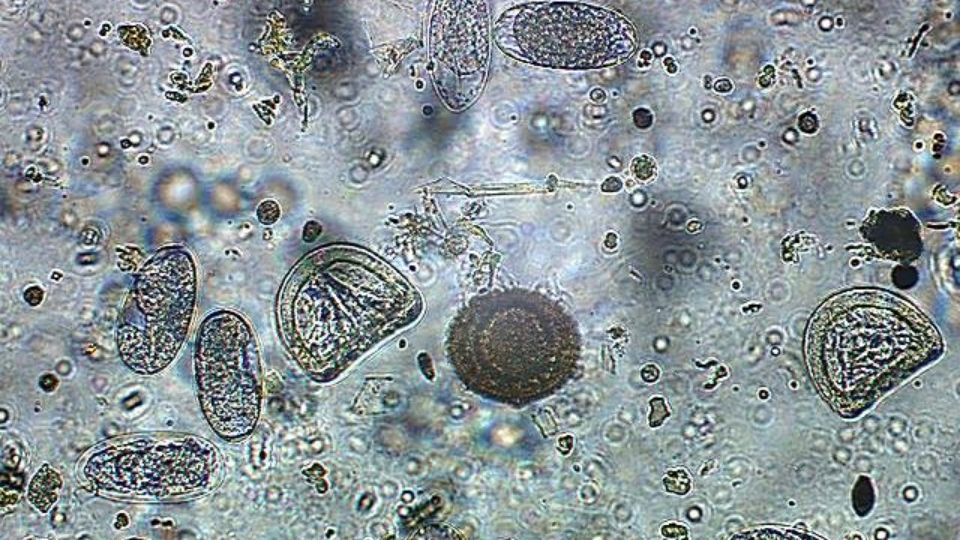
An accurate way to diagnose navicular is by doing a palmar digital nerve block. By anesthetizing a specific region of the foot, veterinarians can assess more accurately where the pain is coming from. Horses with navicular syndrome will “have a decrease in lameness (by) 90% after perineural anesthesia of the palmar digital nerves.”2 Diagnostic imaging through radiography is the most common way to evaluate changes in the navicular bone (Figure 2). Radiographs also help show the hoof pastern axis alignment, medial-lateral imbalance, joint spacing, and palmar angles. This can be used to assess degeneration and incorrect angles that will affect the balance of the hoof.
Magnetic resonance imaging (MRI) is becoming more popular and invaluable when assessing bones and soft tissue at the same time. MRIs can provide a detailed picture of pathological changes, support the choice for optimal treatment, and facilitate the prognosis for the horse’s return to use and performance.4
Another diagnostic tool used is thermography, which shows heat in the horse’s limb and can indicate blood flow to that region. Horses with navicular syndrome won’t show an increase in blood flow to the palmar aspect of the hoof after exercise like normal horses, which can confirm vascular alteration and compromise.2
Treating Navicular Syndrome
Correct Anatomical Abnormalities
The first goal in treating navicular cases is to correct any hoof abnormalities or imbalances. Low underrun heels and long toes increase the load on the deep digital flexor tendon; for every one-degree decrease in hoof angle, the strain on the deep digital flexor tendon is increased by 4%.4 About 21% of horses with navicular have a broken back hoof pastern axis, which accentuates the forces on the navicular bone.2 The most common recommendation is to raise the heels with a 2–4 degree wedge and roll the toe of the shoe to facilitate easier breakover.2 Increasing the angle of the heel will create a straighter hoof pastern axis alignment, which will produce the appropriate amount of force on the navicular bone by the deep digital flexor tendon.5 Adding a bar shoe can also reduce the forces on the navicular region by providing additional support to the heel.3 Almost all cases recommend using proper hoof care as a fundamental treatment for navicular syndrome.
Offer Medication
Nonsteroidal anti-inflammatory drugs (NSAIDs) are used in conjunction with other treatments to alleviate pain and inflammation. Phenylbutazone is the most commonly used NSAID and provides temporary comfort for navicular cases. Corticosteroid injection of the distal interphalangeal joint or the navicular bursa is another medical option for treating inflammation associated with navicular syndrome.
Perform Surgery
A surgical procedure used for navicular syndrome is a palmar digital neurectomy (PDN). This procedure involves cutting or removing the palmar digital nerve on each side of the foot. It should be used only as a last resort since it eliminates the sensation of the hoof by disconnecting the nerves to the palmar third portion of the foot. Catastrophic injury to both horse and rider has been reported after horses return to high levels of competition following a PDN. Additionally, there can be many complications with the procedure, including neuromas and rupture of the DDFT.6
Provide Physical Therapy
Ultimately, the last category of treatment involves physical therapy. Rest is essential when inflammation is present to prevent additional stress on internal structures, although complete confinement is not necessary. Thirty minutes of light daily exercise is recommended to help increase blood flow to the foot, but only after proper shoeing. Additionally, the horse may require a change in daily use, requiring a much lighter workload.
Conclusion
Navicular syndrome can be a serious ailment, especially since its complete origin is still unknown and is often chronic and progressive. Although the prognosis is poor to guarded in most cases, with correct hoof balance and proper medical treatment to help alleviate pain, reduce lameness, and minimize the degenerative process, navicular syndrome may be managed, thus allowing horses to maintain their current level of activity and competition for several years. However, over months to years of treatment, most horses diagnosed with navicular syndrome will reach a point and become unresponsive to medical treatment.6
Photo Credit
Figure photos were provided by Karl H. Hoopes and require attribution.
Footnote References
1 Waguespack, W., & Hanson, R. (2010). Navicular syndrome in equine patients: Anatomy, causes and diagnosis. Surgical Views, 8(2), 1–14.
2 Turner, T. A. (1989). Diagnosis and treatment of navicular syndrome in horses. Veterinary Clinics of North America: Equine Practice, 5(1), 131–144.
3 Schoonover, M. J., Jann, H. W., & Blaik, M. A. (2005). Quantitative comparison of three commonly used treatments for navicular syndrome in horses. American Journal of Veterinary Research, 66(7), 1247–1251.
4 Mieszkowska, M., Adamiak, Z., Mieszkowska, M., Holak, P., & Wolinska, K. (2016). Magnetic resonance imaging provides a detailed perspective of navicular syndrome in horses. Praca Oryginala, 72(5), 298–302.
5 Waguespack, W., & Hansons, R. (2011). Treating navicular syndrome in equine patients. Surgical Views, 11(3), 1–10.
6 Belknap, J. K. (2015). Navicular disease in horses. In Merck Veterinary Manual. https://www.merckvetmanual.com/musculoskeletal-system/lameness-in-horses/navicular-disease-in-horses
Published June 2023
Utah State University Extension
Peer-reviewed fact sheet
Authors
Karl Hoopes, DVM USU Equine Extension Specialist; Kylie Stephens, USU Equine Science and Management
Related Research