Opioid Use Disorder (OUD) and Pregnancy in Utah

Over the past twenty years, opioid use during pregnancy has become much more common (Haight et al., 2018). Opioids may be prescribed for pain management or the treatment of an opioid use disorder (OUD). For example, methadone or buprenorphine are medications recommended for pregnant women with OUD. Opioid use may also include misusing prescription painkillers or using illicit drugs such as heroin. Regardless of the nature of opioid use, it is important for pregnant women to know how opioid use can impact their pregnancy and what treatment options are available.
Basic Facts
- Drug overdose is the number one cause of death in Utah for women who recently delivered a baby, and 77% of these deaths are due to opioids (Smid et al., 2019).
- While babies cannot be “addicted” to opioids because they lack the social factors necessary for an addiction diagnosis, babies exposed to opioids in utero, especially illicit opioids like heroin, have higher risks of poor growth, premature birth, and opioid withdrawal symptoms (Centers for Disease Control [CDC], 2021; Reddy et al., 2017).
- Prenatal care and checking a baby’s health after birth is especially important for parents who use opioids (American College of Obstetrics and Gynecology, 2017; CDC, 2021; Reddy et al., 2017).
- Effective medical treatments for OUD, such as methadone and buprenorphine, can help wom-en have a healthy pregnancy and reduce the risk of health problems for babies compared to babies born to women with untreated OUD (Brogly et al., 2014; CDC, 2021; Jones et al., 2010; Reddy et al., 2017).
Trends
- Between 1999 and 2014, OUD in pregnancy rose at an alarming rate, up over 333% in the United States (1.5 to 6.5 per 1,000 delivery ospitalizations). In Utah, the rate of increase was even greater, up 825% (0.4 to 3.7 per 1,000 delivery hospitalizations) (Haight et al., 2018).
- In a nine-year period between 2005 and 2014, 27 women died of opioid overdose in Utah within a year of giving birth (Smid et al., 2019).
Healthy Outcomes
- With proper medications for opioid use disorder (MOUD) treatment for women during pregnancy, babies are at lower risk of being born too early, too small, or having opioid withdrawal after birth when exposed to opioids during pregnancy (CDC, 2019).
- Mothers who received MOUD were more likely to track their baby’s growth and health appropriately and maintain custody than mothers with untreated OUD (Berg et al., 2008).
- Mothers receiving MOUD during pregnancy are more likely to have a baby with a healthy birth weight and less likely to deliver their baby prematurely (Berg et al., 2008).
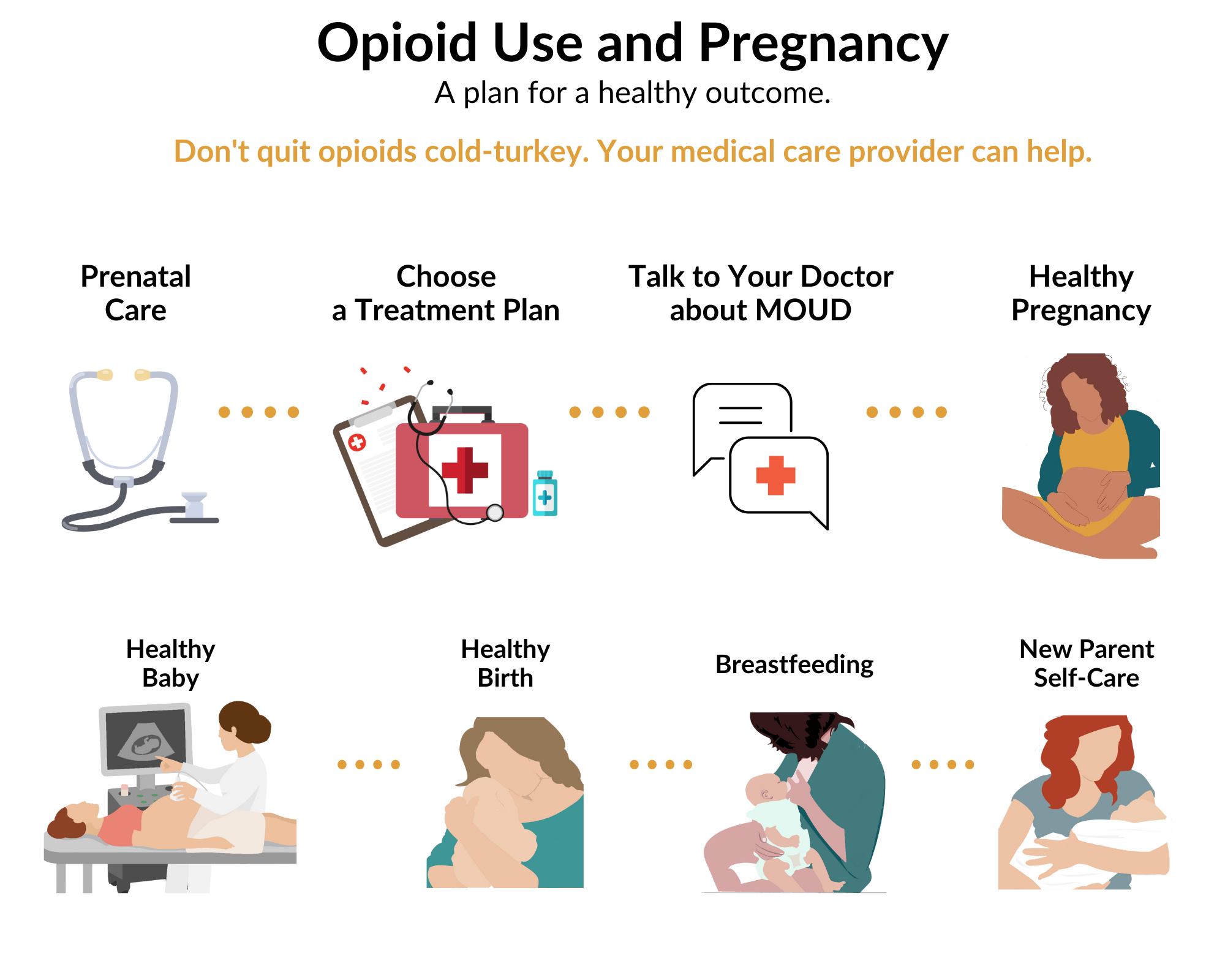
- Establishing and implementing a plan can lead to healthier outcomes for mothers and infants (Figure 1).
Treatment Resources
- Call the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline: 1-800-662-HELP (4357) – free and confidential, 24/7 treatment referral and information, available in English and Spanish.
- Find a provider near you using the SAMHSA Opioid Treatment Program Directory: OTP Directory (samhsa.gov).
- Access Pregnancy Resources for Women and Families from the Utah Department of Health, Maternal and Infant Health Program: https://mihp.utah.gov/opioids.
- Use Resources on Opioid Use During Pregnancy from the Centers for Disease Control and Prevention: https://www.cdc.gov/pregnancy/ opioids/resources.html.
References
- American College of Obstetricians and Gynecologists (ACOG) (2017). Committee opinion no. 711 summary: Opioid use and opioid use disorder in pregnancy. Obstetrics & Gynecology, 130 (2), 488–489. https://doi.org/10.1097/aog.0000000000002229.
- Berg, R. C., Winsvold, A., Kornør, H., Øverland, S., Smedslund, G., Hammerstrøm, K. H., Storetvedt, K., Johnsen, J., Hansen, H., & Tømmervik, K. (2008). Effects of opioid agonist treatment for pregnant opioid dependent women. Kunnskapssenteret No. 31−2008. Norwegian Knowledge Centre for the Health Services, The Norwegian Directorate of Health. https://www.ncbi.nlm.nih.gov/books/NBK464917/pdf/Bookshelf_NBK464917.pdf.
- Brogly, S. B., Saia, K. A., Walley, A. Y., Du, H.M., & Sebastiani, P. (2014). Prenatal buprenorphine versus methadone exposure and neonatal outcomes: Systematic review and meta-analysis. American Journal of Epidemiology, 180 (7), 673–686. https://doi.org/10.1093/aje/kwu190.
- Centers for Disease Control and Prevention (CDC) (2021). About opioid use during pregnancy. U.S. Department of Health and Human Services. https://www.cdc.gov/pregnancy/opioids/basics.html.
- Haight, S. C., Ko, J. Y., Tong, V. T., Bohm, M. K., & Callaghan, W. M. (2018). Opioid use disorder documented at deliv-ery hospitalization — United States, 1999–2014. Morbidity and Mortality Weekly Report, 67 (31), 845–849. http://dx.doi.org/10.15585/mmwr.mm6731a1.
- Jones, H. E., Kaltenbach, K., Heil, S. H., Stine, S. M., Coyle, M. G., Arria, A. M., O’Grady, K. E., Selby, P., Martin, P. R., & Fischer, G. (2010). Neonatal abstinence syndrome after methadone or buprenorphine exposure. New England
Journal of Medicine, 363 (24), 2320–2331. https://doi.org/10.1056/NEJMoa1005359. - Reddy, U. M., Davis, J. M., Ren, Z., & Greene, M. F. (2017). Opioid use in pregnancy, neonatal abstinence syn-drome, and childhood outcomes [Workshop presentation]. In Opioid Use in Pregnancy, Neonatal Abstinence Syn-drome, and Childhood Outcomes Workshop. Obstetrics & Gynecology, 130 (1), 10–28. https://doi.org/10.1097/AOG.0000000000002054.
- Smid, M. C., Stone, N. M., Baksh, L., Debbink, M. P., Einerson, B. D., Varner, M. W., & Clark, E. A. S. (2019). Pregnancy-associated death in Utah. Obstetrics & Gynecology, 133 (6), 1131–1140. https://doi.org/10.1097/
aog.0000000000003279.
Utah State University Extension
Peer-reviewed fact sheet
Download PDF
Authors
Saralyn Margetts, Erin Fanning Madden, Lauran Hymas, Katie Zaman, Gabriela Murza, Suzanne Prevedel, and Sandra H. Sulzer
Related Research




