Cross-Cultural Collaborations for Addressing Opioid Use Disorders in Utah

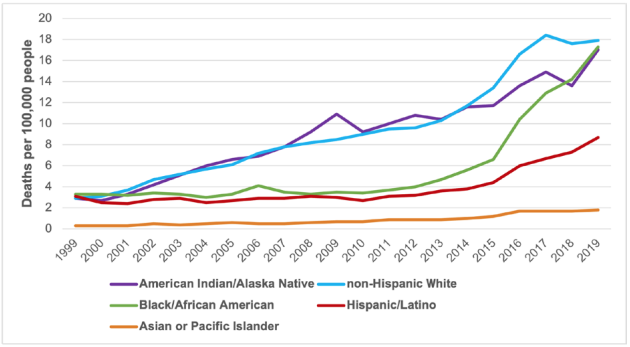
American Indian and Alaska Native (AI/AN) communities have experienced rising rates of opioid overdose death over the past two decades. The opioid overdose death rate involving any opioid for the AI/AN population rose from 2.9 per 100,000 people in 1999 to 17.0 in 2019. This number surpasses the national rate of 15.2 deaths per 100,000 in 2019 (CDC, 2020). Fatal opioid overdose rates are higher in this period among AI/AN populations than rates among Hispanic and Asian American populations, and in 2019 data, AI/AN populations are just below both Black/African American and non-Hispanic White population death rates (Figure 1) (CDC, 2020). These trends may vary in their magnitude across regions. For example, consider the opioid overdose deaths per 100,000 among AI/AN populations from 2015–2019: Minnesota, 50.6; Arizona, 14.7; and Utah, 18.7. The Utah opioid overdose death rate for AI/AN populations was well over the state rate of 14.2 per 100,000 for this five-year period, signaling the need for statewide efforts tailored to American Indian communities.

Cultural Adaptation vs. Cultural Centering
A process of adapting and reorienting effective interventions for opioid use disorders and opioid overdose can improve intervention dissemination to tribal communities. Methods for changing interventions to fit the cultures of local communities include “cultural centering” and “cultural adaptation,” each of which describes steps for altering interventions to suit communities.
Cultural adaptation refers to changes to interventions that consider culture and context in ways that are compatible with the norms, values, and meanings of the intended audience (Bernal, Jiménez-Chafey, & Rodríguez, 2009).
Cultural centering is a related but slightly different approach, which focuses on including Indigenous People as co-creators of interventions (Gittelsohn et al.,2020). Cultural centering focuses more explicitly on the value of Indigenous knowledge and on reciprocal learning between people promoting effective interventions and the knowledge and power within tribal communities (Belone et al., 2017; Dutta, 2007) (Table1).
Effective Interventions
Efforts to address opioid use disorders and opioid overdose should include syringe distribution programs, overdose education and naloxone trainings, and treatment using medications for opioid use disorder. While individuals of any race, ethnicity, and geography can benefit from these services, interventions that do not meaningfully consider the norms, values, and priorities of local communities may inadvertently contribute to underutilized services and even lead to inequities in resources and health outcomes(Baumann & Cabassa, 2020; Dickerson et al., 2020; Rathod et al., 2018).
Table 1. Approaches to Cross-Cultural Collaboration
| Cultural adaptationa | Cultural centeringb |
|---|---|
|
Adjusting effective interventions:
|
Leveraging culture as a powerful recource when creating interventions:
|
aBernal & Sáez‐Santiago, 2006; Heim et al., 2019
bBelone et al., 2017; Dutta, 2007
Cultural Humility
All forms of cross-cultural collaboration require team members to embrace “cultural humility.” Cultural humility emphasizes engagement in lifelong learning and critical self-reflection about actions and thinking. It also emphasizes the recognition of power imbalances and requires a commitment to changing these imbalances. Finally, it requires institutional accountability, where institutions like universities and healthcare organizations must also model these principles (Tervalon & Murray-García, 1998). Institutional accountability may entail a variety of approaches to modeling cultural humility.
Cultural Humanity
Cultural humility encompasses ways of thinking and behaving that reimagine how people in power approach marginalized groups of people.
Institutional Accountability
Institutions like universities, healthcare organizations, and local governments must also model the principles of cultural humility in order to engage in effective cross-cultural collaboration.
For example, including members of Indigenous groups in powerful positions as decision-makers within organizations and funding community-based participatory research in which tribal or other communities are not “research subjects” and instead operate as equal partners in conducting studies with universities and foundations. When working with marginalized populations, it is essential for researchers and service providers to remain culturally humble in order to assure interventions are altered in ways that truly respond to community culture and priorities.
Collaboration in Action
The Utah State University Tribal and Rural Opioid Initiative (TROI) utilized insights from cultural adaptation and cultural centering research to create opioid use disorder-related outreach and education interventions for Utah’s tribal communities. The TROI team includes members from the Ute Indian Tribe living on the Uintah and Ouray Reservation in rural northeastern Utah and non-tribal rural and urban collaborators from Utah and other states. Academic experts on the TRIO team initially developed interventions for nonspecific audiences and then altered and reoriented each intervention (Table 2).
Table 2. Steps Taken During the Cross-Cultural Collaboration Process
| Step | Process details |
|---|---|
| 1. Create preliminary content. |
Academic experts develop initial intervention elements for nonspecific populations:
|
| 2. Present preliminary content. |
Trainings and summit delivered to nonspecific populations, with tribal community members in attendance. |
| 3. Engage in focus froups. |
Focus groups and surveys with tribal community members used to adjust nonspecialized |
| 4. Edit intervention intensively. |
Materials altered to target tribal communities:
|
| 5. Deliver revised intervention to tribal communities. |
Trainings and summit delivered by tribal community members and offered to tribal community audiences. |
*Consultation with tribal community-based TROI members throughout.
Through this process, the TROI team developed approaches for delivering evidence-based resources to address adverse opioid-related health outcomes with and for members of Utah’s tribal communities. This cross-cultural collaboration developed naloxone trainings for tribal community members that included free naloxone distribution, harm reduction trainings for substance use disorder counselors practicing in Indigenous communities, and a four-day annual summit providing substance use and general wellness education for tribal communities (the Rural and Tribal Opioid Summit). The summit was attended by 99 tribal community members. Additionally, 16 naloxone trainings were delivered to tribal community-based groups and community members, including those attending the summit and other presentations made to general audiences in tribal communities. A total of 374 people attended the naloxone trainings, with representation from 90 tribal communities, including five of the eight tribes in Utah. A professional training for substance use treatment professionals working with tribal populations is also in its final stages of development and will be made available to tribal communities for further use in 2021.
Summary
Cross-cultural collaboration allows for more effective interventions for opioid use disorder among tribal communities. Practicing cultural humility, incorporating Indigenous knowledge, and amplifying Indigenous voices are crucial to the cross-cultural collaboration process. This process can ensure that interventions that address opioid use disorder meet the needs of tribal communities.
For more information about the Utah State University Tribal and Rural Opioid Initiative Resource Center or to request a naloxone training, please contact the TROI Resource Center webpage at https://extension.usu.edu/healthwellness/healthequity/troi/about.
References
- Baumann, A. A. & Cabassa, L. J. (2020). Reframing implementation science to address inequities in healthcare delivery. BMC Health Services Research 20(1), 190. doi:10.1186/s12913-020-4975-3
- Belone, L., Orosco, A., Damon, E., Smith-McNeal, W., Rae, R., Sherpa, M. L., Myers, O. B., Omeh, A. O., & Wallerstein, N. (2017). The piloting of a culturally centered American Indian family prevention program: A CBPR partnership between Mescalero Apache and the University of New Mexico. Public Health Reviews 38(1), 1–13. doi:10.1186/s40985-017- 0076-1
- Bernal, G. & Sáez‐Santiago, E. (2006). Culturally centered psychosocial interventions. Journal of Community Psychology, 34(2), 121–132. https://doi.org/10.1002/jcop.20096
- Bernal, G., Jiménez-Chafey M. I., & Rodríguez, M. (2009). Cultural adaptation of treatments: A resource for considering culture in evidence-based practice. Professional Psychology: Research and Practice, 40(4), 361–368. doi:10.1037/A0016401
- Centers for Disease Control and Prevention (CDC) (2020). CDC WONDER online database multiple cause of death files, 1999–2019. U.S. Department of Health and Human Services. http://wonder.cdc.gov/mcd-icd10.htm
- Dickerson, D., Baldwin, J. A., Belcourt, A., Belone, L., Gittelsohn, J., Kaholokula, J. K., Lowe, J., Patten, C. A., & Wallerstein, N. (2020). Encompassing cultural contexts within scientific research methodologies in the development of health promotion interventions. Prevention Science, 21(1), 33–42. doi:10.1007/s11121-018-0926-1
- Dutta, M. J. (2007). Communicating about culture and health: Theorizing culture-centered and cultural sensitivity approaches. Communication Theory, 17(3), 304–328. https://doi.org/10.1111/j.1468-2885.2007.00297.x
- Gittelsohn, J., Belcourt, A., Magarati, M., Booth-LaForce, C., Duran B., Mishra, S. I., Belone, L., & Blue Bird Jernigan, V. (2020). Building capacity for productive indigenous community - University partnerships. Prevention Science, 21(1), 22–32. doi:10.1007/s11121-018-0949-7
- Heim, E., Shehadeh, M. H., van’t Hof, E., & Carswell, K. (2019). Cultural adaptation of scalable interventions. In A. Maercker, E. Heim, & L. J. Kirmayer (Eds.), Cultural clinical psychology and PTSD (pp. 201–218). Hogrefe Publishing.
- Rathod, S., Gega, L., Degnan, A., Pikard, J., Khan, T., Husain, N., Munshi, T., & Naeem, F. (2018). The current status of culturally adapted mental health interventions: a practice-focused review of meta-analyses. Neuropsychiatric Disease and Treatment 2018, 14, 165–178. doi:10.2147/NDT.S138430
- Tervalon, M. & Murray-García, J. (1998). Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. Journal of Health Care for the Poor and Underserved, 9(2), 117–125. doi:10.1353/hpu.2010.0233
Utah State University Extension
Peer-reviewed fact sheet
Download PDF
Authors
Michelle Q. Chapoose, Cassandra Manning, Erin Fanning Madden, Katie Zaman, Claire Warnick, Suzanne Prevedel, and Sandra H. Sulzer

