Cognitive Behavioral Therapies for the Management of Chronic Pain

What is Chronic Pain?
Chronic pain is pain that lasts longer than six months and may continue even after illnesses or injuries have healed (Cleveland Clinic, 2017). Pain signals in the nervous system can remain active for several years if they are altered in the spinal cord, becoming stronger than they normally would or should be (Reichling & Levine, 2009). Chronic pain can also occur without illness or injury (National Institute of Neurological Distorders and Stroke, 2019). Fortunately, many evidence-based strategies for managing chronic pain are available to ease the discomfort.
Chronic pain is one of the most common reasons individuals seek medical care, with 10%-40% of the population reporting chronic pain at any given time (Nickel & Raspe, 2001). Chronic pain can lead to a decrease in mobility, reduced quality of life, opioid dependence, anxiety, depression, and poorer perceived health (Nickel & Raspe, 2001).
Why Is Chronic Pain Difficult to Treat?
Identifying the source of the pain can prove difficult for healthcare providers and patients alike (Clauw, 2015). Diagnostic tools to help identify sources of pain can include both non-invasive (e.g., physical examination, imaging, questionnaires) and invasive (e.g. blood tests, nerve conduction studies) procedures, which are used to understand or treat symptoms (Clauw, 2015).
In addition, pain can look different for different people. Pain can be both the cause or the response to changes in functioning referred to as a symptom cycle (Lorig, 2015). See Figure 1 below that shows the symptom cycle. The cycle of chronic pain involves a decrease in physical activity, which can lead to negative emotions, then avoidance, followed by distress, which leads back to chronic pain. The symptom of pain creates changes in experience, which leads to changes in thinking and behavior, which then exacerbates or makes the pain worse in a negative spiral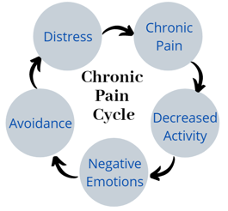
Figure 2.
While the use of prescription opioids can be a valuable treatment option for individuals with acute pain and cancer pain (Rosenquist et al., 2019), the risks of use with chronic pain have led to the pursuit of alternatives. Opioids have both a pain-reducing effect and create a rapid feeling of relief, which can lead to substance use disorder or inappropriate use and potential overdose (Volkow & McLellan, 2016). Additionally, the effect of opioids lessens over time and people don’t get the same relief they once had from their medication dose.
Recommended Ways to Manage Chronic Pain*
The U.S. Centers for Disease Control and Prevention (CDC) lists six effective non-opioid options for patients dealing with chronic pain (Centers for Disease Control and Prevention, 2020), with cognitive approaches that focus on our thoughts high on the list. These options include:
- Over-the-counter medications for pain. Medications used to treat chronic pain include over-the-counter pain medications like acetaminophen (TYLENOL®) and ibuprofen (ADVIL®, MOTRIN®).
- Cognitive behavioral therapy. A psychological, goal-directed approach in which patients learn how to modify physical, behavioral, and emotional triggers (or thoughts) of pain and stress.
- Exercise therapies. Physical therapy, exercise, and weight loss.
- Medications for depression or seizures. Medications that act on the nervous system like gabapentin, certain antidepressants, and topical medications.
- Intervention therapies. Injections, surgery, etc.
- Other therapies such as acupuncture or massage.
What Are Cognitive Therapies and How Do They Help with Pain?
Cognitive behavioral therapy (CBT), biofeedback, relaxation therapy, and individual and group therapy have proven effective in the treatment of chronic pain (Hofmann, et al., 2012). Cognitive therapies for chronic pain teach active problem-solving approaches to cope with chronic pain and the many ways it can affect quality of life. Some key cognitive therapies for chronic pain include:
- Relaxation training
- Cognitive restructuring
- Mindfulness
- Behavioral activation
- Pacing
All cognitive therapies for pain help to break the symptom cycle linking unhelpful thoughts, negative emotions, and increased pain. By altering thoughts, individuals can directly reduce negative feelings that lead to avoidance and more pain (Murphy et al., 2014).
Cognitive Behavioral Therapy for Pain
CBT is a specialized form of therapy that can be used alone or as a component within a comprehensive treatment plan for chronic pain. CBT is traditionally led by a licensed therapist and can be conducted in individual or group therapy. CBT for pain is structured, goal-directed, and uses a problem-solving approach with three components:
- Education
- Behavioral skills training
- Cognitive skill training
CBT helps patients identify the negative thoughts that influence feelings and behaviors (see Figure 2 below) and teaches skills to change those thoughts and behaviors. CBT works by helping individuals understand their thoughts, the impulses they trigger, and teaches skills to replace negative thought cycles with healthy interpretations or coping skills (Gatchel, McGeary, McGeary, & Lippe, 2014).
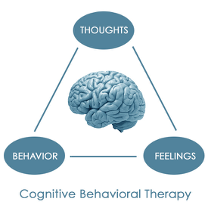
Figure 2.
The process or CBT allows individuals the cognitive flexibility to reduce the way their thoughts feed into the pain symptom cycle. This means individuals can learn to act, rather than react, as they choose how to deal with their pain. These coping skills help individuals with chronic pain to change their awareness of pain and manage pain symptoms.
Does CBT Work for Pain
Cognitive therapies have proven effective in helping individuals achieve some level of relief from their pain symptoms. Although CBT is considered the “gold standard,” it is often underused (Garland & Howard, 2018; Hofmann et al., 2012; National Academy of the Sciences, 2011). CBT for chronic pain has many benefits, including improved daily functioning, quality of life, and it works well for a variety of chronic pain conditions (Morley, Eccleston, & Williams, 1999). CBT has been shown to be effective even when used in web-based formats, lowering distressing thoughts about pain and decreasing negative substance-related behaviors (Guarino et al., 2018). An additional benefit of CBT is that it is a time-limited therapy. While CBT is learned through a process of collaboration from the therapist and the patient, it can then be used continuously without additional treatments for ongoing pain relief (Murphy et al., 2014). Additionally, CBT is an evidence-based treatment that can support pain management with or without the use of prescription opioid medications (e.g., by psychologists; Yaugher et al., 2020).
Do I Need to See a Therapist to Practice CBT?
Yes, to engage in evidence-based CBT you must see a licensed therapist (e.g., social worker, counselor, psychologist). While CBT is a proven approach to reduce pain, other cognitive approaches for managing pain can be learned without going to therapy. To get started, there are many self-help books and approaches for learning CBT as well as other pain management techniques. A brief list is below.
Cognitive Behavioral Resources**
- Beck Institute CBT for pain resources: https://beckinstitute.org/%D1%81ondition/chronic-pain/
- Association for Behavioral and Cognitive Therapies approved resources: http://www.abct.org/SHBooks/
- National Alliance on Mental Illness list of Self-Help Cognitive Therapy resources: https://www.nami.org/Blogs/NAMI-Blog/November-2016/Discovering-New-Options-Self-Help-Cognitive-Behav
Other Cognitive Resources (Mindfulness and Relaxation)**
- American Mindfulness Research Association (AMRA): https://goamra.org/
- Loyola, University of Maryland Counseling Center, Relaxation Resources: https://www.loyola.edu/department/counseling-center/students/relaxation
- UC San Diego Health (Center for Mindfulness, Videos About Stress and Mindfulness): https://health.ucsd.edu/specialties/mindfulness/resources/Pages/video.aspx
- UC San Diego Health (Center for Mindfulness, Guided Audio Files to Practice MBSR): https://health.ucsd.edu/specialties/mindfulness/programs/mbsr/Pages/audio.aspx
Summary
Because of the recent opioid overdose epidemic in the country, and the contraindications for opioid use for chronic pain, it is important to identify safer and more effective treatments for managing pain symptoms. CBT is an evidence-based, effective treatment to reduce pain symptoms and improve quality of life. CBT is a safer alternative to opioids and can be a cost-effective way to reduce pain.
References
- Centers for Disease Control and Prevention. (2020). Know your options. Retrieved April 6, 2020 from https://www.cdc.gov/drugoverdose/patients/options.html
- Clauw, D. J. (2015). Diagnosing and treating chronic musculoskeletal pain based on the underlying mechanism(s). Best Practice & Research: Clinical Rheumatology, 29(1), 6–19. doi:10.1016/j.berh.2015.04.024
- Cleveland Clinic. (2017). Acute pain versus chronic pain. Retrieved January 26, 2019 from https://my.clevelandclinic.org/health/articles/12051-acute-vs-chronic-pain
- Garland, E. L., & Howard, M. O. (2018). Mindfulness-based treatment of addiction: Current state of the field and envisioning the next wave of research. Addiction Science Clinical Practice, 13(1), 14. doi:10.1186/s13722-018-0115-3
- Gatchel, R. J., et al. (2014). Interdisciplinary chronic pain management: Past, present, and future. American Psychology, 69(2), 119–130. doi:10.1037/a0035514
- Guarino, H., et al. (2018). Web-Based cognitive behavior therapy for chronic pain patients with aberrant drug-related behavior: Outcomes from a randomized controlled trial. Pain Medicine, 19(12), 2423-2437. doi:10.1093/pm/pnx334
- Hofmann, S. G., et al. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36(5), 427–440. doi:10.1007/s10608-012-9476-1
- Jean-Christophe. (n.d.). Iceberg. Pexels.com. Retrieved June 23, 2020 from https://www.pexels.com/photo/iceberg-in-body-of-water-2575005/
- Lorig, K. (2015). Chronic disease self-management program: Insights from the eye of the storm [Opinion]. Frontiers in Public Health, 2(253). doi:10.3389/fpubh.2014.00253
- Morley, S., et al. (1999). Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain, 80(1-2), 1–13. doi:10.1016/s0304-3959(98)00255-3
- Murphy, J., et al. (2014). Cognitive behavioral therapy for chronic pain among veterans: Therapist manual.Washington, D.C.: U.S. Department of Veterans Affairs.
- National Academy of the Sciences. (2011). Relieving pain in America: A blueprint for transforming prevention, care, education, and research (22553896). Washington D.C.: National Academy of Sciences. doi:10.17226/13172
- National Institute of Neurological Distorders and Stroke, N. (2019). Retrieved March 27, 2019 from https://www.ninds.nih.gov/Disorders/All-Disorders/Chronic-pain-Information-Page
- Nickel, R., & Raspe, H. H. (2001). Chronic pain: Epidemiology and health care utilization. Der Nervenarzt, 72(12), 897–906. doi:10.1007/s001150170001
- Reichling, D. B., & Levine, J. D. (2009). Critical role of nociceptor plasticity in chronic pain. Trends in Neurosciences, 32(12), 611-618. doi:10.1016/j.tins.2009.07.007
- Volkow, N. D., & McLellan, A. T. (2016). Opioid Abuse in Chronic Pain--Misconceptions and Mitigation Strategies. New England Journal of Medicine, 374(13), 1253–1263. doi:10.1056/NEJMra1507771
- Yaugher, A. C., Bench, S. W., Meyers, K. J., & Voss, M. W. (2020). How psychologists can impact the opioid epidemic. Professional Psychology: Research and Practice, 51(1), 85–93. https://doi.org/10.1037/pro0000287
Disclaimer
*Always consult a doctor when considering treatment or management of a medical condition.
**Please note that all of the resources provided are for educational purposes and Utah State University (USU) does not specifically endorse their services. Cognitive behavioral and other cognitive resources are intended to provide information, not to treat chronic pain or other mental health concerns. USU does not control the websites or books referenced above.
Authors
Ashley Yaugher, Maren Voss, Kira Swensen, Alise Williams Condie
Related Research






