Nutrition and Chronic Pain

The internet is full of information about anti-inflammatory diets, foods and supplements that are claimed to prevent or alleviate chronic pain. Dietary advice is essential for those that struggle with chronic pain to improve diets and ultimately decrease pain (Arranz et al., 2010). However, it’s important to note that research showing the impact of specific foods on health and the immune system is currently limited, therefore these claims should be interpreted with caution (Elma et al., 2020; Harvard Health, 2018). This fact sheet will cover 1) how inflammation effects chronic pain and 2) how eating a well-balanced diet may play a role in reducing inflammation which can contribute to chronic pain.
Explained: Inflammation & Chronic Pain
Inflammation is the body's natural and protective response to injury and harm. Inflammation plays an important role in healing; however chronic low-level inflammation may cause pain and damage to healthy cells (Nelms & Sucher, 2019)
Many individuals with chronic pain have elevated levels of proinflammatory cytokines, which are small proteins released by immune cells in the body that promote inflammation (Rondanelli et al., 2018). Having elevated levels of proinflammatory cytokines is a normal response to injury, infection, and/or irritation, as inflammation protects and promotes healing (Rondanelli, et al., 2018). Typically, as the body heals, the inflammation subsides as well. However, sometimes inflammation continues. Overtime, this can damage healthy cells and organs, causing constant pain in muscles, tissues and joints. Chronic inflammation is often suggested as one of the underlying causes of various chronic pain conditions such as fibromyalgia, chronic low back pain, rheumatoid arthritis, myofascial pain syndrome, and osteoarthritis (Elma et al., 2020). Chronic inflammation may also increase the risk for developing other chronic conditions like heart disease (Nelms & Sucher, 2019). Research suggests that eating a balanced diet has a large positive effect in reducing chronic pain (Brian et al., 2019)
Role of Nutrition with Chronic Pain
Many studies have shown that an integrative lifestyle, combined with pharmaceutical approaches are far more beneficial in treating chronic pain than just medication (Philpot & Johnson, 2019, p.335). Nutrition is one of the key components in everyone’s lifestyle that can benefit the many effects that chronic pain has on the body. Diet quality, nutrient density and weight management are all involved in changing pain physiology (Field et al., 2020).
Balanced nutrition is required for all cells in the body to function optimally, with immune cells being no exception. Immune cells must receive the nutrients they need to perform their job. Without appropriate nutrition, negative changes in the immune system may occur and may increase the risk of chronic low-grade inflammation (Childs et al., 2019). There is increasing concern that modern lifestyle and diet has resulted in the promotion of ongoing, low-grade inflammation (Childs et al., 2019, p.2). The Western diet is generally characterized by a high intake of sugar, fats and sodium, and a low intake of whole grains, fiber, micronutrients, and other bioactive molecules such as polyphenols and omega 3 polyunsaturated fatty acids (Brian et al., 2019; Childs et al., 2019). Diets of highly processed foods, high in saturated fats, trans fats or sugar have been positively linked with persistent low-grade inflammation (Barbaresko et al., 2013; Harvard Health, 2018).
However, with different dietary choices, diet can have a positive effect on chronic inflammation and chronic pain. Most studies suggest that eating an overall balanced diet provides sufficient nutrients to help keep the immune cells working well. For example, fruits and vegetables contain phytonutrients which are natural and active compounds that may help protect against inflammation and reduce musculoskeletal pain (Gordon, 2019, section 2; Towery et al., 2018). In addition, some polyunsaturated fatty acids, such as omega-3 fatty acids, and monounsaturated fatty acids may aid in the regulation of inflammation (Bjørklund et al., 2019). Lastly, foods rich in a group of antioxidants known as polyphenols may have an anti-inflammatory effect that soothe and prevent painful flare-ups(Childs et al., 2019; Elma et al., 2020). These foods include many of the staples of the Mediterranean diet, such as whole fruits (especially berries), dark green leafy vegetables, nuts, legumes, and whole grains (Childs et al., 2019; Elma et al., 2020; Lahoz et al., 2018). See Figure 1 for tips on eating more healthy fats, whole grains, fruits, and vegetables, and protein.
An example of antioxidants working within a specific chronic pain illness is fibromyalgia (Bjorklund et al., 2018). Fibromyalgia is a common chronic pain disorder that is characterized by long-lasting muscle pain and tenderness throughout your body (Fibromyalgia, 2014). Bjorklund et al. (2018), found that following a diet rich in antioxidants improved fibromyalgia symptoms such as musculoskeletal, and nerve pain (p. 532). Fibromyalgia is just one of the many chronic pain disorders that nutrition can have a positive impact on.
What does a well-balanced diet look like?
- All foods in moderation. Remember that all foods can fit into a healthy diet. There is no need to eliminate any food group or favorite treat, unless instructed by a physician for medical reasons. Eating healthy or eating a well-balanced diet simply means mostly eating a variety of foods that will nourish your body. It does not mean eating "perfectly" or rigidly. No matter what the media or other influencers may say, there is no one best way of eating and there is no perfect food. Eating should be enjoyable and give your body the energy it needs to thrive (LeFort et al., 2015).
- Listen to your body. Give yourself permission to eat a snack or meal when you are hungry or need energy. Eat slowly to determine when your body has had enough. Be mindful of what your body is telling you when you are eating and focus on the experience (LeFort et al., 2015).
- Choose food first! While taking a variety of supplements and vitamins may seem convenient, it is important to remember to eat those nutrients in their most natural form (LeFort et al., 2015). Taking too many supplements may lead to toxic levels of certain vitamins or minerals. Following a well-balanced diet will give the body the nutrients it needs in the correct amounts. Supplements should be used to fill in nutrient gaps and not as a main source of nutrition. Talk with a doctor or dietitian to determine which supplements are right for you (LeFort et al., 2015).
Role of Water with Chronic Pain
Water is an essential nutrient and aids all processes in the body. Some preliminary research has found that not drinking enough may increase pain sensitivity. However, the exact process of how water effects chronic pain is not fully understood. Regardless, drinking sufficient amounts of water is important in managing chronic pain (Bear et al., 2016)
The water Dietary Reference Intake for men is 15 ½ cups (3.7 liters) of total water daily and for women it is about 11 ½ cups (2.7 liters) of water daily (Institute of Medicine, 2005). Generally, foods consumed throughout the day account for about 20% of the total water needed. Fluids (water and other beverages) make up the remaining 80%. It is recommended that men drink about 13 cups (3.0 liters) of fluid (with a special emphasis on water) and that women drink around 9 cups (2.2 liters) of fluid daily to ensure adequate intake (Institute of Medicine, 2005).
It should be noted that certain medical conditions and age may alter how much water the body needs (older adults and younger children may have differing fluid needs). Check with your doctor or dietitian to see if your fluid needs are different.
One indicator to see if the body is getting enough water is to check urine color. Light yellow or colorless urine generally indicates hydration. Dark yellow or brown urine generally indicates dehydration. However, certain medications or supplements may also impact urine color. Check with your doctor if you continue to have dark colored urine.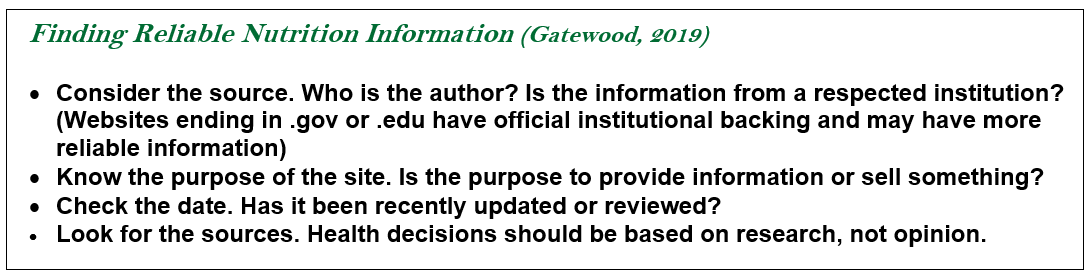
(Institute of Medicine, 2005). Other indicators of hydration or dehydration include thirst, fatigue, and mental alertness (Institute of Medicine, 2005).
Looking for more information?
Use the text box below as a guide to help in determining accurate and reliable sources of nutrition information. As always, a doctor or registered dietitian is a good source of nutrition information.
|
Include fruits and vegetables with every meal |
Choose Whole Grains |
Select Healthy Fats |
Have Protein |
|
1. Eat a variety of both. Use fruits and vegetables to make your plate colorful. |
1. Look at the nutrition facts label/ingredient list for words like "whole-grain" or "100% whole-grain". Not all brown grains are whole! |
1. Use monounsaturated fats like olive, safflower, sunflower, canola, peanut and avocado oils. |
1.Choose leaner protein foods, such as poultry or lean cuts of beef and pork |
|
2. Fill ½ your plate with both. |
2. Eat a variety of whole grains |
2. Eat omega-3 rich foods like nuts, fatty fish, flaxseed, and chia seeds. |
2. Minimize highly processed meats like deli meat, bacon, and sausage. |
|
3. All forms count! (fresh, frozen, canned, dried, steamed, roasted) |
3. Try and make ½ of all grains eaten whole grains |
3. Minimize highly processed foods that contain partially hydrogenated oils and high amounts of saturated fat. |
3. Enjoy meatless meals with other high protein foods like legumes, eggs, yogurt, and tofu. |
References
- Institute of Medicine (2005).Dietary reference intakes: For water, potassium, chloride, and sulfate. The National Academies Press. https://doi.org/10.17226/10925
- Arranz, L. I., Canela, M. A., Rafecas, M. (2010). Fibromyalgia and nutrition, what do we know?. Rheumatology International 30, 1417-1427. https://doi.org/10.1007/s00296-010-1443-0
- Barbaresko, J., Koch, M., Schulze, M.B., & Nöthlings, U. (2013). Dietary pattern analysis and biomarkers of low-grade inflammation: a systematic literature review. Nutrition Reviews, 71(8), 511-27. https://doi.org/10.1111/nure.12035
- Bear, T., Philipp, M., Hill, S., & Mündel, T. (2016). A preliminary study on how hypohydration affects pain perception. Psychophysiology, 53(5), 605–610. https://doi.org/10.1111/psyp.12610
- Bjørklund, G., Aaseth, J., Doşa, M. D., Pivina, L., Dadar, M., Pen, J. J., & Chirumbolo, S. (2019). Does diet play a role in reducing nociception related to inflammation and chronic pain?. Nutrition, 66, 153–165. https://doi.org/10.1016/j.nut.2019.04.007
- Bjørklund, G., Dadar, M., Chirumbolo, S., & Aaseth J. (2018). Fibromyalgia and nutrition: Therapeutic possibilities?. Biomedicine & Pharacotherapy 103, 531-538. https://doi.org/10.1016/j.biopha.2018.04.056
- Brain, K., Burrows, T. L., Rollo, M. E., Chai, L. K., Clarke, E. D., Hayes, C., Hodson, F. J., & Collins, C. E. (2018). A systematic review and meta-analysis of nutrition interventions for chronic noncancer pain. Journal of human nutrition and dietetics, 32(2), 198–225. https://doi.org/10.1111/jhn.12601
- Childs, C. E., Calder, P. C., & Miles, E. A. (2019). Diet and Immune Function. Nutrients, 11(8),1-9. https://doi.org/10.3390/nu11081933
- Elma, Ö., Yilmaz, S.T., Deliens, T., Coppieters, I., Clarys, P., Nijs, J., & Malfliet, A. (2020). Do nutritional factors interact with chronic musculoskeletal pain?: A systematic review. Journal of Clinical Medicine, 9(3), 1-23. https://doi.org/10.3390/jcm9030702
- Fibromyalgia. (2014, July). National Institute of Arthritis and Musculoskeletal and Skin Diseases. Retrieved Feburary 5, 2021, from https://www.niams.nih.gov/health-topics/fibromyalgia
- Gatewood, J. (2019, January 14). Good or bad?: Finding reliable nutrition information on the web. Spend Smart. Eat Smart. https://blogs.extension.iastate.edu/spendsmart/2019/01/14/good-or-bad-finding-reliable-nutrition-information-on-the-web/
- Gordon, B. (2019, July 25). Can Diet Help with Inflammation?. Eat Right.org. https://www.eatright.org/health/wellness/preventing-illness/can-diet-help-with-inflammation
- Harvard Health. (2018, July) Can diet heal chronic pain?. Harvard Health Publishing. https://www.health.harvard.edu/pain/can-diet-heal-chronic-pain
- Lahoz, C., Castillo, E., Mostaza, J. M., De Dios, O., Salinero-Fort, M. A., Gozales-Alegre, T., Garcia-Iglesias, F., Estirado, E., Laguna, F., Sanches, V., Savin, C., Lopez, S., Cornejo, V., De Burgo, C., Garces, C. (2018). Relationship of the adherence to a mediterranean diet and its main components with CRP levels in the Spanish population. Nutrients, 10(3), 1-9.
https://doi.org/10.3390/nu10030379 - LeFort, S. M., Webster, L., Lorig, K., Holman, H., Sobel, D., Laurent, D., Gonzalez, V., & Minor, M. (2015). Living a healthy life with chronic pain. Bull Publishing Company.
- Nelms, M., Roth, S. L., & Sucher, K. P. (2019). Nutrition Therapy & Pathophysiology. Cengage Learning.
- Philpot, U., Johnson, M. I. (2019). Diet therapy in the management of chronic pain: better diet less pain?. Pain Management 9(4), 335-338. https://doi.org/ 10.2217/pmt-2019-0014
- Raphael, W., & Sordillo, L. M. (2013). Dietary polyunsaturated fatty acids and inflammation: The role of phospholipid biosynthesis. International Journal of Molecular Sciences, 14(10), 21167–21188. https://doi.org/10.3390/ijms141021167
- Rondanelli, M., Faliva, M. A., Miccono, A., Naso, M., Nichetti, M., Riva, A., Gurriero, F., Gregori, M. D., Peroni, G., & Perna, S. (2018) Food pyramid for subjects with chronic pain: Foods and dietary constituents as anti-inflammatory and antioxidant agents. Nutrition Research Reviews 31(1), 131-151. https://doi.org/10.1017/s0954422417000270
- Towery, P., Guffery, S., Stroup, K., Saucedo, S., Taylor. (2018) Chronic musculoskeletal pain and function improve with a plant-based diet. Complementary Therapies in Medicine, 40, 64-69. https://doi.org/10.1016/j.ctim.2018.08.00
Authors
Elise Withers, BS; Mateja R. Savoie-Roskos PhD, MPH, RD; Riley Samples, BS; Maren Wright Voss, ScD
Related Research

