Vape Prevention: How Teachers Can Help

What Is Vape?
Electronic cigarette (e-cigarette) use is an emerging problem among youth, and is commonly referred to as ”vaping” (CATCH, 2020; Selekman, 2019). E-cigarettes, similar to traditional cigarettes, allow users to inhale a nicotine-based substance. 
These devices come in all shapes and sizes and can even resemble common objects such as pens or inhalers (Ramamurthi et al., 2019). E-cigarettes also go by several names such as vape, mod, pen, electronic nicotine delivery system (ENDS), and JUUL.
Although there are numerous types of e-cigarette devices, they all have the same core pieces and functions. They consist of a battery, microprocessor (what turns on the device), heater (also known as the atomizer), and tank or cartridge, (what stores the e-liquid; CATCH, 2020; Krishnan-Sarin et al., 2019). These devices come either prefilled with or can be manually filled with e-liquid flavoring. When a user activates the device by inhaling through the mouthpiece, the e-liquid is heated and undergoes chemical changes to produce an aerosol (i.e., pressurized substance; Callahan-Lyon, 2014; CATCH, 2020;). This aerosol is often referred to and mistaken as a harmless “vapor” when in fact it is not, and can cause significant harms. Figure 1 below represents a breakdown of common e-cigarette components (adapted from the U.S. Department of Health and Human Services [HHS], n.d.).
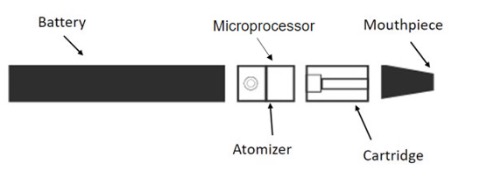
Figure 1: A visual representation of some common e-cigarette components including a battery, microprocessor, atomizer, cartridge, and mouthpiece (adapted from the U.S. Department of HHS, n.d.).
Not "Just Water Vapor"
When the aerosol produced by e-cigarettes is mistakenly called “water vapor,” it implies that it is safe and harmless, which it is not. Unlike water vapor, aerosol produced by e-cigarettes contain particles, chemicals, and elements that may cause a variety of negative health effects when inhaled (CATCH, 2020; Walley et al., 2019). Some of the currently known substances found in e-liquid and the effects on the body are listed in table below.
| Ingredient Name | Effects on the Body |
|---|---|
|
Nicotine (Also used in insecticides) |
Alters the brain and habit-forming properties |
|
Propylene Glycol (Also used in antifreeze) |
Lactic acidosis and seizures |
|
Diacetyl (Flavoring chemical) |
Asthma, chronic pulmonary obstructive disorder, and popcorn lung |
|
Acrolein (Component of smoke) |
Dyslipidemia (i.e., elevated cholesterol) and is a respiratory irritant |
|
Formaldehyde (Also used to preserve cadavers) |
Eye, nose, and throat irritant; cancer-causing agent |
|
Heavy Metals (Such as nickel, lead, and cadmium) |
Damages lungs, kidneys, brain; cancer-causing agent |
(Bein & Leikauf, 2011; Bhat et al., 2019; Catanzaro & Smith, 1991; CATCH, 2020; Clapp et al., 2017; Conklin et al., 2010; Dani & Balfour, 2011; Jensen et al., 2015; Kehrer et al., 2000; Rose, 2017; Vape Danger, n.d.; Zosel et al., 2010)
Nicotine Harms Students
False advertising leads people to believe that e-liquids do not contain nicotine. However, one study found that nearly 99% of e-liquids contain nicotine, even when they were labeled as “nicotine-free" (Marynak et al., 2017). Manufacturing companies aren’t required to list all ingredients in the e-liquids, misleading what's actually in the product (Cobb et al., 2020). Students unaware of this could be using products they believe to be nicotine free, when they actually aren’t.
Nicotine is known for its habit-forming properties (Dani & Balfour, 2011). Youth are at an increased risk of these habit-forming properties as the human brain is still developing until the approximate age of 25 years (CATCH, 2020; Dwyer et al., 2009). The use of nicotine before this age physically alters the brain and the synapse connections formed, increasing the likelihood of habitual use, future substance use disorders, marijuana use, and binge drinking (CATCH, 2020; Evans-Polce et al., 2020).
E-liquids have a high concentration of nicotine (Goniewicz et al., 2014). For example, the nicotine contained in a single JUUL pod (5% nicotine) is equal to the amount contained in an entire pack of 20 cigarettes (Singh et al., 2020). Youth are able to consume e-cigarette aerosols easily and quickly because added flavors suppress the bitterness of nicotine (Leventhal et al., 2020). Alternative methods used in e-cigarette products, such as adding nicotine salts to the top of the e-liquid, produce more nicotine, allowing users to inhale even more nicotine per use (Ramamurthi et al., 2019).
E-cigarettes & Substance Use
Due to the negative consequences of using e-cigarettes, the Center for Disease Control and Prevention (CDC) recommends that youth and young adults never try them and to quit if they are using them (CDC, 2020). Studies have shown that youth who vape are 6.8 times more likely to start smoking cigarettes than non-users (CATCH, 2020; Evans-Polce et al., 2020). In youth, e-cigarettes are considered a gateway substance as they have been known to lead to other substance use such as marijuana and binge drinking (Evans-Polce et al., 2020).
Associated Lung Illnesses
Lung Illnesses include asthma or bronchitis as well as more severe lung issues (Stalgaitis et al., 2020). E-cigarette use among youth is known for its association with certain lung illnesses. The flavoring chemical, diacetyl, is safe to ingest but not inhale through the lungs like it is through e-cigarette use (CATCH, 2020; Vas et al., 2019). Research shows that inhalation of diacetyl can cause Chronic Obstructive Pulmonary Disorder (COPD), popcorn lung (shortness of breath), and even increase asthma (Rose, 2017; Vape Danger, n.d.). Vitamin E acetate, an ingredient found in dab pens (a type of e-cigarette for marijuana use) is also known for its negative effects on the lungs (CATCH, 2020; Boudi et al., 2019). For example, in 2019, 13 Utah hospitals admitted 60 patients due to vaping, where 98% of the patients had respiratory symptoms and 55% were placed in intensive care (Blagev, at el., 2019). Furthermore, research suggests that youth who use e-cigarettes are 5 times more likely to be exposed to and diagnosed with COVID-19, compared to youth who do not use e-cigarettes (Gaiha et al., 2020). Additionally, the risk of contracting COVID-19 is 7 times greater for youth who smoke both e-cigarettes and traditional cigarettes (CATCH, 2020; Gaiha et al., 2020).
Signs & Health Impacts of Student Vape Use
Students should be taught about the side effects of e-cigarette use, and these side effects should not be dismissed as “normal teenage behavior.” Cognitive symptoms include difficulty concentrating as a result of nicotine dependence or withdrawal symptoms (CATCH, 2020; HHS, 2016). The use of products with nicotine may also have long-term effects on attention and memory (Stalgaitis et al., 2020). Youth may also show behavioral changes such as mood changes, anxiety, and irritability (CATCH, 2020; Popova et al., 2021). Physical symptoms include mouth sores, bloody nose, and dry mouth (Burt & Li, 2020; CATCH, 2020; Yang et al., 2020). Ensure youth learn about these and other side effects so they understand the dangers of e-cigarette use.
As teachers, you may find it helpful to be able to identify signs of use and ways youth can hide the devices. Below is a table that provides some common examples:
| Identifying Signs of Use: |
|
| Possible Hiding Places: |
|
(California Department of Public Health, n.d.; CATCH, 2020; Ramamurthi et al., 2019; Schillo et al., 2020; Stalgaitis et al., 2020)
What Can Teachers Do?
Teachers have the unique opportunity to both monitor and influence student behaviors at school (Sallis et al., 2015) and have been specifically identified by the U.S. Surgeon General as crucial stakeholders to address youth e-cigarette use (HHS, 2016). Teachers can be effective in this role by:
- Staying informed and up-to-date on e-cigarette harms and products to be able to identify new products and inform students of potential risks of use (Schillo et al., 2020).
- Advocating for educational resources and curricula (such as CATCH My Breath) to be disseminated at school to provide this information, better intervene, and prevent e-cigarette use (Schillo et al., 2020).
- Advocating for comprehensive school tobacco policies that specifically include vaping and JUUL prevention to ensure a tobacco-free space at school (Schillo et al., 2020).
- Helping students understand the harms of e-cigarette use (HHS, 2016).
There are several resources available including lesson plans, additional education on e-cigarettes, and trainings on how to identify if youth are using e-cigarettes. Below is a brief list of resources with additional information to learn more or get started.
Online Resoucres
|
Be Epic, Escape the Vape Resources for parents, teachers and youth |
CATCH My Breath Free lesson plans, PowerPoints, and worksheets |
|
Scholastic Lessons, activities and digital tools |
Rethink Vape Factual information about e-cigarettes |
|
The Real Cost Factual information about e-cigarettes |
Truth Initiative Research and information about e-cigarettes https://truthinitiative.org/research-resources/topic/emerging-tobacco-products?subtopic%5B68%5D=68 |
Here are a few resources to give your students for help or ways to quit.
Resources for Students to Quit
- Text 'QUIT' to 47848
- Text 'DITCHVAPE" to 88709
- 1-800-QUIT-NOW
- https://truthinitiative.org/thisisquitting
*Please note that all of the resources provided are for educational purposes and Utah State University (USU) does not specifically endorse their services. Resources are intended to provide information, not to treat substance use/vape use or other mental health concerns. USU does not control the websites or books referenced above.
References
- Bein, K., & Leikauf, G. D. (2011). Acrolein – A pulmonary hazard. Molecular Nutrition & Food Research, 55(9), 1342-1360. https://doi.org/10.1002/mnfr.201100279
- Bhat, D., Chittoor, H., Murugesh, P., Basavanna, P. N., & Doddaiah, S. (2019). Estimation of occupational formaldehyde exposure in cadaver dissection laboratory and its implications. Anatomy & Cell Biology, 52, 419-425. https://doi.org/10.5115/acb.19.105
- Blagev, D. P., Harris, D., Dunn, A. C., Guidry, D. W., Grisson, C. K., & Lanspa, M. J. (2019). Clinical presentation, treatment, and short-term outcomes of lung injury associated with e-cigarettes or vaping: A prospective observation cohort study. Lancet, 394(10214), P2073-P2083. https://doi.org/10.1016/S0140-6736(19)32679-0
- Boudi, F. B., Patel, S., Boudi, A., & Chan, C. (2019). Vitamin E acetate as a plausible cause of acute vaping-related illness. Cureus, 11(12), e6350. https://dx.doi.org/10.7759%2Fcureus.6350
- Burt, B., & Li, J. (2020). The electronic cigarette in youth and young adults: A practical review. Journal of the American Academy of Physician Assistants, 33(3), 17-23. https://doi.org/10.1097/01.JAA.0000654384.02068.99
- California Department of Public Health. (n.d.). Parent resources. Flavors Hook Kids, Tobacco Free CA. Retrieved December 10, 2020 from https://www.flavorshookkids.org/parent-resources/
- Callahan-Lyon, P. (2014). Electronic cigarettes: Human health effects. Tobacco Control, 23(Suppl 2), ii36-ii40. https://doi.org/10.1136/tobaccocontrol-2013-051470
- Catanzaro, J. M., & Smith Jr., J. G. (1991). Propylene glycol dermatitis. Journal of the American Academy of Dermatology, 24(1), 90-95 https://doi.org/10.1016/0190-9622(91)70018-W
- CATCH. (2020). CATCH My Breath Vaping Prevention Program: State of the Union of the Youth Vaping Epidemic and Introduction to an Evidence-Based Prevention Program. Retrieved December 4, 2020 from https://letsgo.catch.org/courses/take/ToT-catch-my-breath/texts/20244840-community-trainer-master-presentation
- Centers for Disease Control and Prevention [CDC]. (2020, November 27). Outbreak of lung injury associated with the use of e-cigarette, or vaping, products. Retrieved January 27, 2021, from https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html
- Clapp, P. W., Pawlak, E. A., Lackey, J. T., Keating, J. E., Reeber, S. L., Glish, G. L., & Jaspers, I. (2017). Flavored e-cigarette liquids and cinnamaldehyde impair respiratory innate immune cell function. American Journal of Physiology Lung Cellular and Molecular Physiology, 313(2), L278-L292. https://doi.org/10.1152/ajplung.00452.2016
- Cobb, N. K., & Solanki, J. N. (2020). E-cigarettes, Vaping Devices, and Acute Lung Injury. Respiratory Care,66(5), 713-718. https://doi.org/10.4187/respcare.07733
- Conklin, D. J., Barski, O. A., Lesgards, J. F., Juvan, P., Rezen, T., Rozman, D., Prough, R. A., Vladykovskaya, E., Liu, S., Srivastava, S., & Bhatnagar, A. (2010). Acrolein consumption induces systemic dyslipidemia and lipoprotein modification. Toxicology and Applied Pharmacology, 243(1), 1-12. https://doi.org/10.1016/j.taap.2009.12.010
- Dani, J. A., & Balfour, D. J. K. (2011). Historical and current perspective on tobacco use and nicotine addiction. Trends in Neurosciences, 34(7), 383-392. https://doi.org/10.1016/j.tins.2011.05.001
- Dwyer, J. B., McQuown, S. C., & Leslie, F. M. (2009). The dynamic effects of nicotine on the developing brain. Pharmacology & Therapeutics, 122(2), 125-139. https://doi.org/10.1016/j.pharmthera.2009.02.003
- Evans-Polce, R. J., Veliz, P., Boyd, C. J., & McCabe, S. E. (2020). Initiation patterns and trends of e-cigarette and cigarette use among US adolescents. Journal of Adolescent Health, 66(1), 27-33. https://doi.org/10.1016/j.jadohealth.2019.07.002
- Gaiha, S. M., Cheng, J., & Halpern-Felsher, B. (2020). Association between youth smoking, electronic cigarette use, and COVID-19. Journal of Adolescent Health, 67(4), 519-523. https://doi.org/10.1016/j.jadohealth.2020.07.002
- Goniewicz, M. L., Knysak, J., Gawron, M., Kosmider, L., Sobczak, A., Kurek, J., Prokopowicz, A., Jablonska-Czapla, M., Rosik-Dulewska, C., Havel., C., & Jacob, P. (2014). Levels of selected carcinogens and toxicants in vapor from electronic cigarettes. Tobacco Control, 23(2), 133-139. https://doi.org/10.1136/tobaccocontrol-2012-050859
- Jensen, R. P., Luo, W., Pankow, J. F., Strongin, R. M., & Peyton, D. H. (2015). Hidden formaldehyde in e-cigarette aerosols. New England Journal of Medicine, 372(4), 392-394. https://doi.org/10.1056/NEJMc1413069
- Kehrer, J. P., & Biswal, S. S. (2000). The molecular effects of acrolein. Toxicological Sciences, 57(1), 6-15. https://doi.org/10.1093/toxsci/57.1.6
- Krishnan-Sarin, S., Jackson, A., Morean, M., Kong, G., Bold, K. W., Camenga, D. R., Cavallo, D. A., Simon, P., & Wu, R. (2019). E-cigarette devices used by high-school youth. Drug and Alcohol Dependence, 194, 395-400. https://doi.org/10.1016/j.drugalcdep.2018.10.022
- Leventhal, A. M., Mason, T. B., Cwalina, S. N., Whitted, L., Anderson, M. K., & Callahan, C. E. (2020). Flavor and nicotine effects on e-cigarette appeal in young adults: Moderation by reason for vaping. American Journal of Health Behavior, 44(5), 732-743. https://doi.org/10.5993/AJHB.44.5.15
- Marynak, K, L., Gammon, D. G., Rogers, T., Coats, E. M., Singh, T., & King, B. A. (2017). Sales of nicotine containing electronic cigarette products: United States, 2015. American Journal of Public Health, 107(5), 702-705. https://doi.org/10.2105/AJPH.2017.303660
- Popova, L., Fairman, R. T., Akani, B., Dixon, K., & Weaver, S. R. (2021). “Don’t do vape, bro!” A qualitative study of youth’s and parents’ reactions to e-cigarette prevention advertisements. Addictive Behaviors, 112, 106565. https://doi.org/10.1016/j.addbeh.2020.106565
- Ramamurthi, D., Chau, C., & Jackler, R. K. (2019). JUUL and other stealth vaporisers: Hiding the habit from parents and teachers. Tobacco Control, 28(6), 610-616. http://dx.doi.org/10.1136/tobaccocontrol-2018-054455
- Rose, C. S. (2017). Early detection, clinical diagnosis, and management of lung disease from exposure to diacetyl. Toxicology, 388, 9-14. https://doi.org.10.1016/j.tox.2017.03.019
- Sallis, J. F., Owen, N., & Fisher, E. (2015). Ecological models of health behavior. In Glantz, K., Rimer, B. K., Viswanath, K. (Eds), Health Behavior: Theory, Research, and Practice (Vol. 5, pp. 43-64). San Francisco, CA: Jossey-Bass.
- Schillo, B. A., Cuccia, A. F., Patel, M., Simard, B., Donovan, E. M., Hair, E. C., & Vallone, D. (2020). JUUL in school: Teacher and administrator awareness and policies of e-cigarettes and JUUL in US middle and high schools. Health Promotion Practice, 21(1), 20-24. https://doi.org/10.1177%2F1524839919868222
- Selekman, J. (2019). Vaping: It's all a smokescreen. Pediatric Nursing, 45(1), 12-15.
- Singh, S., Windle, S. B., Filion, K. B., Thombs, B. D., O’Loughlin, J. L., Grad, R., & Eisenberg, M. J. (2020). E-cigarettes and youth: Patterns of use, potential harms, and recommendations. Preventive Medicine, 133, 106009. https://doi.org/10.1016/j.ypmed.2020.106009
- Stalgaitis, C. A., Djakaria, M., & Jordan, J. W. (2020). The vaping teenager: Understanding the psychographics and interests of adolescent vape users to inform health communication campaigns. Tobacco Use Insights, 13, 1179173X20945695. https://doi.org/10.1177/1179173X20945695
- U.S. Department of Health and Human Services [HHS]. (n.d.). Know the risks e-cigarettes & young people: Get the facts. U.S. Department of Health and Human Services, Office of the U.S. Surgeon General, & Centers for Disease Control and Prevention, Office on Smoking and Health [graphic adapted from]. Retrieved from https://e-cigarettes.surgeongeneral.gov/getthefacts.html
- U.S. Department of Health and Human Services [HHS]. (2016). E-cigarette use among youth and young adults. A report of the Surgeon General. Atlanta, GA. Retrieved from https://www.cdc.gov/tobacco/data_statistics/sgr/e-cigarettes/pdfs/2016_sgr_entire_report_508.pdf
- Vape Danger. (n.d.) Vaping health risks. Vape Danger. Retrieved December 7, 2020 from https://www.vapedanger.com/health-risks/
- Vas, C. A., Porter, A., & McAdam, K. (2019). Acetoin is a precursor to diacetyl in e-cigarette liquids. Food and Chemical Toxicology, 133, 110727. https://doi.org/10.1016/j.fct.2019.110727
- Walley, S. C., Wilson, K. M., Winickoff, J. P., & Groner, J. (2019). A public health crisis: Electronic cigarettes, vape, and JUUL. Pediatrics, 143(6), e-20182741. https://doi.org/10.1542/peds.2018-2741
- Yang, I., Sandeep, S., & Rodriguez, J. (2020). The oral health impact of electronic cigarette use: A systematic review. Critical Reviews in Toxicology, 50(2), 97-127. https://doi.org/10.1080/10408444.2020.1713726
- Zosel, A., Egelhoff, E., & Heard, K. (2010). Severe lactic acidosis after an iatrogenic propylene glycol overdose. Pharmacotherapy, 30(2), 219. https://doi.org/10.1592/phco.30.2.219
Authors
Jordyn Oman, Health and Wellness Prevention Coordinator; Jenna Hawks, Health and Wellness Prevention Coordinator; Hailey Judd, Health and Wellness Coordinator; Ashley Yaugher, Professional Practice Assistant Professor; Cris Meier, Community Resource and Economic Develpment Specialist; Christina Pay, Extension Assistant Professor
Related Research





